If you are an athlete, there is a good chance you have heard of medial tibial stress syndrome, or “shin splints.” This condition is very common among runners and other athletes who participate in sports that involve a lot of running. In this blog post, we will discuss the causes, symptoms, and treatment of medial tibial stress syndrome. We will also provide information on how to prevent this condition from occurring.
Contents
What Is Medial Tibial Stress Syndrome?
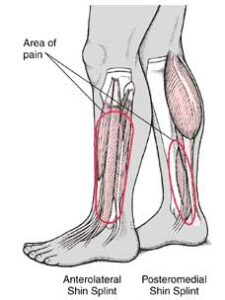
Medial tibial stress syndrome (MTSS) is a condition that causes pain and tenderness along the inside of the shinbone (tibia), specifically where the bone meets the muscle. MTSS is also referred to as shin splints and is a common overuse injury among runners and other athletes.
Medial tibial stress syndrome (MTSS) is a condition that causes pain and inflammation in the shin, specifically in the medial tibialis posterior (MTP) muscle. The MTP muscle is located on the inside of the lower leg, just behind the shinbone (tibia). MTSS is often referred to as “shin splints.”
What Are The Symptoms?
The most common symptom of medial tibial stress syndrome is pain along the inside of your shinbone (tibia). This pain is usually worse when you exercise, and it gets better with rest. You might also feel a dull ache in your shinbone after exercising.
There are various symptoms of MTSS including:
- Pain and tenderness along the inside border of the shinbone (tibia), typically during or after exercise
- Swelling in the affected area
- Stiffness and difficulty flexing the foot upwards
If you experience any of these symptoms, it is important to see a doctor or healthcare provider to rule out other possible causes of shin pain, such as a stress fracture.
What Are the Causes of Medial Tibial Stress Syndrome?

MTSS is caused by overuse of the lower leg muscles and tendons. It is typically caused by overuse of the muscles and tendons that attach to the tibia. This can occur from:
Repeated impact activities
Such as running or jumping, can lead to medial tibial stress syndrome. This is because these activities put repeated stress on the bones, muscles, tendons, and ligaments in your leg.
Overuse
Doing too much activity without giving your body enough time to recover can also lead to medial tibial stress syndrome. This is especially true if you’re not used to the activity or if you’re doing it wrong.
Improper shoes
Wearing shoes that don’t fit well or provide enough support can also lead to medial tibial stress syndrome. For instance, shoes that are too tight can put extra pressure on the muscles and tendons in your leg, while shoes that don’t have enough support can cause your feet to roll inward (overpronation), which puts stress on the tibia.
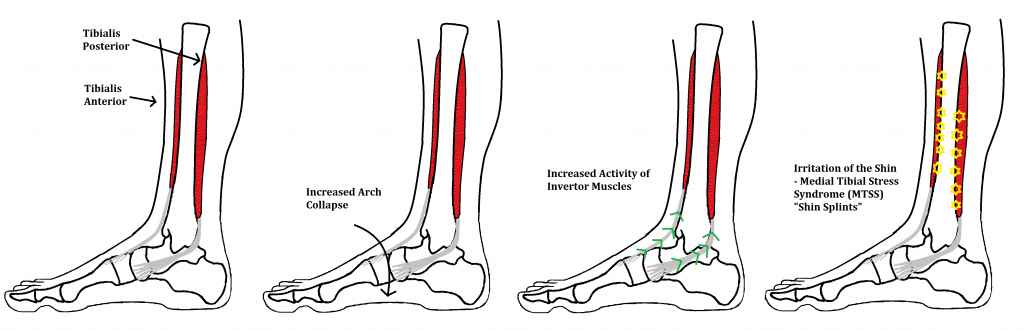
Abnormal biomechanics
If your feet roll inward too much when you walk or run (a condition called overpronation), it can put stress on the tibia. For instance, the tibia rotates inward and the knee collapses inward when you have overpronation. This excessive inward rotation can lead to medial tibial stress syndrome.
Trauma
You may get medial tibial stress syndrome if you’ve had a direct blow to your shin or other trauma to the area. This is more likely to happen if you already have weakness in the muscles or bones in your lower leg.
Muscle imbalances
Having weaker muscles in your calf or hamstring can also lead to medial tibial stress syndrome because these muscles help support the tibia. For instance, if your calf muscles are weak, they can’t absorb as much shock when you run, which puts more stress on the tibia.
Overpronation
This is when your foot rolls inward too much when you walk or run. This can lead to the shinbone (tibia) not getting the support it needs, which can lead to pain.
Thus these are the causes that lead to medial tibial stress syndrome.
Risk Factors
The risk factors for medial tibial stress syndrome include:
- Repetitive impact activities, such as running, dancing, or playing soccer or tennis
- Having flat feet or unusual foot pronation (rolling inward of the ankle during movement)
- Poor flexibility in the calf muscles and hamstrings
- Wearing shoes that are worn out or don’t fit properly
- The sudden increase in mileage or intensity of training
- Running on hard surfaces
Diagnose
There are various diagnose of MTSS. It will include as follows:
Anamnesis
The first step in diagnosing MTSS is to take a detailed medical history from the patient. The clinician will ask questions about the patient’s symptoms, when they started, and what makes them worse or better. They will also inquire about any previous injuries to the lower leg, as well as any other medical conditions the patient may have.
Physical examination
The clinician will then carry out a physical examination of the lower leg. They will look for signs of swelling, tenderness, or redness. They will also assess the range of motion in the ankle and knee and check for any deformities.
Imaging
If the clinician suspects MTSS, they may order imaging tests such as an X-ray, MRI, or CT scan. These can help to rule out other conditions and confirm the diagnosis.
Biomechanical assessment
In some cases, a biomechanical assessment may be carried out. This involves assessing the way the patient walks or runs to see if any abnormal patterns could be contributing to MTSS.
What Are The Treatment options?
The treatment options are as follows:
Rest
This is the most important thing you can do for medial tibial stress syndrome. You need to give your body a chance to heal. Depending on the severity of your symptoms, this may mean taking a few days off from running or cutting back your mileage significantly.
Ice
Applying ice to the affected area can help reduce pain and swelling. For instance, you might try icing for 20 minutes every four hours for two to three days, or until your symptoms resolve. If you ice for too long or too often, it can cause additional inflammation and pain. So be sure to follow the instructions on any over-the-counter ice packs.
Compression
Wearing a compression bandage or wrap can also help reduce swelling. You can buy these bandages at most pharmacies. Be sure to follow the instructions on how tightly to wrap the affected area.
Elevation
Elevating your leg above heart level can also help reduce swelling. Try propping your leg up on a pillow when you’re sitting or lying down. For instance, if you’re sitting in a chair, put your leg up on another chair or stool.
Medications
Over-the-counter medications, such as ibuprofen (Advil, Motrin) or naproxen (Aleve), can help reduce pain and inflammation. Be sure to follow the directions on the package.
If your symptoms are severe, your doctor may prescribe a stronger medication, such as a corticosteroid. Corticosteroids can be taken orally (by mouth) or injected into the affected area.
Stretching and strengthening exercises
Once your symptoms have started to improve, you can begin doing exercises to stretch and strengthen the muscles and tissues around your shin. This will help prevent medial tibial stress syndrome from coming back.
Orthotics
If you have flat feet or high arches, wearing orthotics in your shoes can help to reduce stress on your shins. For people with medial tibial stress syndrome, orthotics can also help to prevent over-pronation, which is a condition in which your feet roll too far inward when you walk. For people with medial tibial stress syndrome, orthotics can help to:
- relieve pain
- reduce inflammation
- improve healing
If you are considering orthotics, be sure to talk to your doctor or a certified orthotist to find out if they are right for you.
Massage
Getting a massage can help to relieve pain and improve blood flow to the affected area. For instance, a 2013 study found that massage reduced pain and improved function in people with MTSS. Another small study from 2014 showed that massage may also help to improve blood flow and reduce inflammation in the area around the shinbone. If you’re interested in trying massage for MTSS, you can see a licensed massage therapist.
Shockwave therapy
This is a newer treatment option that uses sound waves to stimulate healing in the tissues around your shin. It’s thought to be effective in treating medial tibial stress syndrome, but more research is needed. For example, one study found that people who had shockwave therapy along with physical therapy had less pain and better function after six weeks than those who just did physical therapy.
Platelet-rich plasma injections
This treatment involves taking some of your blood, spinning it in a centrifuge to concentrate the platelets, and then injecting the resulting “platelet-rich plasma” into your shin. The platelets help to stimulate healing. For instance, a 2019 study of 71 people with medial tibial stress syndrome found that those who received platelet-rich plasma injections had significantly less pain after 6 weeks than those who didn’t receive the injections.
Surgery
In severe cases, surgery may be necessary to release the affected muscles or tendons. This is usually a last resort, as it can lead to complications and a longer recovery time. For instance, one study found that those who underwent surgery for medial tibial stress syndrome had a significantly higher rate of re-injury and longer recovery times than those who treated the condition with non-surgical methods.
If you think you might have medial tibial stress syndrome, it’s important to see a doctor so they can diagnose the condition and recommend the best treatment for you. With proper treatment, most people make a full recovery and can get back to their normal activity level.
Conclusion
It may be concluded that medial tibial stress syndrome is a condition that can be effectively managed with a combination of treatments, including physical therapy, ice, and anti-inflammatory medication. In some cases, surgery may be necessary to correct the underlying problem. With proper treatment, most people with medial tibial stress syndrome can return to their normal activities.
Physical Therapy help patients recover from pain. If you’re experiencing Back pain, Shoulder pain, Knee pain, Neck pain, Elbow pain, Hip pain, or Arthritis pain, a physical therapist at MantraCare can help: Book a physiotherapy session.