Osteomyelitis is a bone infection that affects the osteo-cortex, or the hard outer shell of your bones. The condition can range from mild to life-threatening, and it often requires aggressive treatment to make sure it doesn’t become chronic. This article will discuss osteomyelitis in detail so you can learn how this serious complication develops and what steps you should take if you think you might have osteomyelitis.
Contents
What Exactly is Osteomyelitis?
Osteomyelitis is an infection of the bone. osteo means “bone”, myeloma refers to the spinal cord and nerve roots in your spine that is made up of bone-forming cells called osteoblasts. This can affect any bone, but common sites include the tibia (shin), femur (thigh), and pelvis. Osteomyelitis is an infection of the bone that causes inflammation in one or more areas of your bone tissue.
Osteomyelitis has four stages:
- Acute osteomyelitis: osteomyelitis develops quickly and is very serious.
- Subacute osteomyelitis (osteomyelitis): an infection of the bone, but not as severe as acute osteomyelitis
- Chronic osteomyelitis: a long term inflammation of the bone with limited damage to the bone that can last for months or even years
- Chronic osteomyelitis with a draining sinus: osteomyelitis where the infection has developed into an abscess. The pus collects in your soft tissue and then drains out of your skin through a hole called a sinus tract.
Symptoms and Signs
Osteomyelitis affects roughly 2 out of every 10,000 individuals. The illness affects people of all ages in varying ways. Certain circumstances and behaviors that weaken the immune system raise one’s chance of developing osteomyelitis.
The symptoms and indications of osteomyelitis vary depending on the kind.
They commonly include:
- Swelling, redness, and soreness in the afflicted region are common symptoms of obstetrics. They can be quite severe.
- Irritability, lassitude, or tiredness
- Sweating, chills, and fever are common symptoms of the disease.
- When you get a cut, the blood sometimes goes down and if it goes into an infection, that is bad.
- Swollen ankles, feet, and legs; as well as if you walk differently like limping, can happen.
Chronic osteomyelitis causes few if any, symptoms. They can go undetected for weeks or months at a time, or they might mimic the effects of an injury.
It may be more difficult to get an accurate diagnosis, particularly in the hip, pelvis, or spine.
Osteomyelitis can be difficult to identify because it sometimes causes no symptoms or the symptoms are hard to differentiate from other diseases. This may be particularly true for babies, elderly people, and patients with weakened immune systems.
Osteomyelitis in Children and Adults

Osteomyelitis is usually acute in children. It develops rapidly, is easier to cure, and has a better result than chronic osteomyelitis in most cases. Osteomyelitis most frequently affects the arm or leg bones of youngsters.
Osteomyelitis can be acute or chronic in adults. Chronic osteomyelitis, which persists or recurs despite therapy, is more likely to affect individuals with diabetes, HIV, or peripheral vascular disease. Osteomyelitis affects both the pelvis and vertebrae of the spine in adults either chronically or acutely. It may also affect the upper extremity bones, ribs, sternum, or skull.
When to Consult a Doctor
If you have a high fever and bone pain gets worse, see your doctor. If you’ve been in an area where there has been a lot of rain recently or if you’re recovering from surgery or an accident, get medical attention right away if you notice indications and symptoms of an infection.
Causes of Osteomyelitis
Staphylococcus bacteria are the most common cause of osteomyelitis. Even healthy individuals have staphylococcus on their skin or in their noses.
Bones can be broken or fractured, and germs may enter them in several ways, including:
- The bloodstream is a major highway for pathogens. Bacteria that have spread from other areas of your body, such as pneumonia or a urinary tract infection, can travel via the bloodstream to an open fracture in a bone.
- Extremely sharp wounds can harbor germs deep within your body. The bacteria in such an injury might spread to a nearby bone if it becomes infected. Germs can also get into your body if you break a bone so severely that part of it protrudes through the surface of your skin.
- The use of medical devices, such as hip implants and surgical instruments, can also transmit infections from one patient to the next. During operations to replace joints or mend fractures, direct contact with germs is possible.
other causes which lead to osteomyelitis are –
- Diabetes (osteomyelitis in most instances)
- Sickle cell disease
- HIV or AIDS
- Rheumatoid arthritis
- Intravenous drug use
- drinking large amounts of alcohol
- using Steroids for a long time
These causes may further cause complications when a person might go for surgery for the same.
Risk Factors in Osteomyelitis
As people age, their bones become less resistant to infection. This protection diminishes as you grow older. Other causes that can make your bones more susceptible to osteomyelitis include:
A significant bone break or a deep puncture wound might provide bacteria entry into your bone or nearby tissue. A significant puncture injury, such as an animal bite or a shoe nail piercing through the bottom, might also offer a route for infection.
Broken or damaged bones, as well as replacements, can occasionally create a passageway for germs to enter the bone. Orthopedic prosthetic devices are an infection risk factor.
When blood vessels are damaged or obstructed, your body has difficulty dispersing the infection-fighting cells required to keep a little sickness from growing worse. A minor cut might evolve into a deep ulcer that exposes deep tissue and bone to illness.
Intravenous lines and catheters are in need in certain situations. Medical tubes are used to connect the outside world with your internal organs in several circumstances. However, this tubing can also act as a pathway for germs to enter your body, raising your chances of getting an infection in general, which can cause osteomyelitis.
- Dialysis machine tubing,
- urinary catheters, and
- long-term intravenous tubes are examples of when this sort of tubing is used.
If your immune system is hampered by disease or drug, you have an increased chance of developing osteomyelitis. Your immune system may be suppressed by:
- Cancer treatment
- with poor diabetes management
- Diabetes medications or TNF inhibitors are in need to take.
People who use unsterile needles and do not sterilize their skin before injections or intaking illegal drugs are more likely to get osteomyelitis due to the possibility of viral or bacterial infections.
Diagnosis of Osteomyelitis
The physician will inspect the afflicted area for symptoms of osteomyelitis, such as pain and swelling. They’ll inquire about your medical history, particularly any recent injuries, operations, or infections.
Tests may include the following:
- High white blood cell counts generally indicate an infection.
- A biopsy is an outpatient procedure in which a tiny piece of tissue is removed to see what kind of pathogen – bacterial or fungal – is causing bone infection. This aids in the discovery of an effective cure.
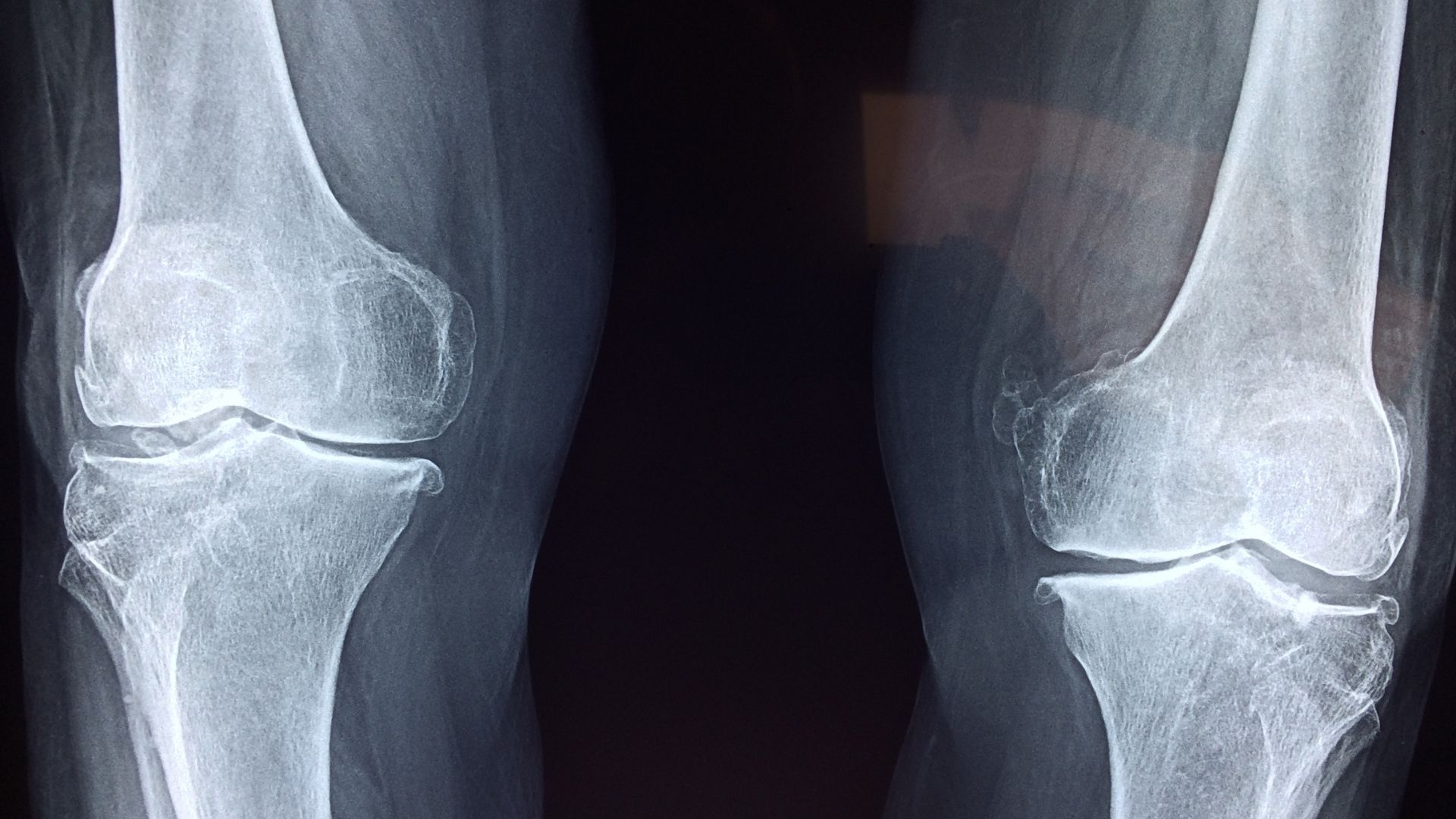
- Any bone damage may be discovered by x-rays, MRIs, or CT scans.
If the injury is recent, an X-ray may not reveal it for two weeks. If the damage has been there for a longer time, more comprehensive MRI or CT imaging is suggested.
Treatment
The goal of treatment is to stop the infection in its tracks and to keep as much function as possible. The majority of people with osteomyelitis are treated using antibiotics, surgery, or both.
Antibiotics assist to control the condition and, in most situations, allow for a surgical cure. People with osteomyelitis frequently receive antibiotics through an IV for several weeks before switching to tablets.
If left untreated, osteomyelitis can lead to the death of the bone or limb. If surgery is not performed within a set time frame, the disease will spread and affect more of the limb. An amputation is always an option in severe or chronic cases of osteomyelitis.
Prevention
The most effective approach to avoid osteomyelitis is to keep your environment clean. Wash any open wound under running water for five minutes, then wrap it in sterile bandages if necessary.
If you have chronic osteomyelitis, make sure your doctor is aware of your medical history so that you may work together to keep the disease in check. If you have diabetes, pay close attention to your feet and notify your physician as soon as possible if you notice an infection.
The sooner you get rid of it, the better. Early treatment in cases of acute osteomyelitis prevents the illness from developing into a long-term problem that needs attention regularly. Aside from the pain and the inconvenience of continuing infections, early management has the best chance for recovery.
Conclusion
Osteomyelitis is a bacterial infection that can happen in any bone. Signs and symptoms vary depending on the type, location, duration, severity, and medical history. The most common symptom is pain or tenderness at the site of infection. You may also have a fever if you are fighting an acute case of osteomyelitis.
If not treated early enough with antibiotics, it could lead to chronic complications such as arthritis or deformity over time.
Prevention includes keeping cuts clean so it doesn’t infect; prompt treatment for wounds that might be dirty or puncture wounds; washing hands often to avoid spreading bacteria from one person to another; wearing shoes when walking outside where there’s animal waste (this way you don’t track in or step on animal waste with bare feet); and keep your house environment, including bathrooms, clean.
Do you want to get rid of diabetes? Join our online diabetes consultation program and reverse your Diabetes naturally through lifestyle changes such as a Personalized Diet plan, Exercise, dieticians, and health coaches.