Many diabetic patients suffer from diabetic foot pain. This is a common complication of diabetes that can lead to serious complications if not treated correctly. However, diabetic foot pain does not have to be an inevitable part of life with diabetes. In this article, we will discuss the signs and symptoms of diabetic foot pain and how one should manage to help you feel better and reduce your chances of developing more serious complications or infections.
Contents
What is Diabetic Foot Pain
Diabetic foot pain is a common diabetic complication marked by pain and nerve damage in the feet. Diabetics often have poor circulation, so blood flow to their feet can reduce which makes it difficult for wounds to heal.
As there isn’t enough oxygenated blood getting through. This wound that won’t close leads to chronic diabetic ulcers.
Although diabetic foot pain is a common form of diabetic complication, it’s also preventable with proper care and precautions so you can manage diabetic foot pain effectively. So what are the warning signs?
Diabetic foot pain will often result in numbness or tingling in your feet at night which goes away once you wake up. You might also feel a sharp or burning pain in your foot that lasts more than three months.
If you have diabetic neuropathy, then the symptoms will be different and may include weakness in muscles of the foot and leg, an unsteady walk, loss of balance control, poor coordination when walking or running, and stiffness of the legs.
Types of Diabetic Foot Pain
Diabetic foot pain is a very common complication of diabetes, occurring in up to 50% of diabetic patients. There are three main types: diabetic neuropathy (nerve damage), Charcot’s joints (joint deformities that occur due to nerve damage), and diabetic ulcers (ulcers on the feet). Depending on which type you have, diabetic foot pain can range from mild to very severe.
Diabetic Foot Pain Neuropathy

It is a diabetic complication that can lead to diabetic foot pain. This type of neuropathy occurs when the small nerves in your feet and legs are damaged by elevated glucose levels over time. Consequently, you may lose feeling or have poor sensation along with an inability to properly control leg movements.
In addition, tight muscles can pull on tendons and cause them to thicken, leading to diabetic foot pain. They may not be aware of the discomfort caused by their shoes. This lack of feeling might lead to more injuries, sores, and blisters.
If left uncontrolled, diabetic neuropathy can lead to serious injuries and infections that may require amputation of your feet or legs.
Diabetic Neuropathies are the most common complication associated with diabetes (90%-95%) If you experience diabetic foot pain it is important not to delay seeking treatment.
A person who does not get treatment for an infection can develop ulcers, as well as gangrene. If a person has gangrene, they might need to have a limb amputated. A doctor may suggest amputation if a person gets gangrene.
Peripheral Neuropathy
The peripheral nervous system is made up of nerves that connect the central (brain and spinal cord) to the rest of your body. This includes your:
- arms and hands
- legs and feet
- face and mouth
- internal organs
The job of these nerves is to communicate information about physical feelings from your body back to your brain. They’re also in charge of keeping your internal functions, such as blood flow and digestion, functioning properly.
Peripheral neuropathy is an inflammation or damage to the peripheral nerves that affect their ability to function properly. This disrupts the nerve’s normal functioning. They might send signals of discomfort when nothing is wrong, or they may not send a pain signal even if you are being harmed. This can be caused by:
- injury
- systemic illness
- infection
- hormonal imbalance
- certain medications
- vitamin deficiency
- an inherited disorder
It may be classified as symmetric or asymmetrical depending on its location. It’s the most prevalent kind of diabetic neuropathy. The feet and legs are affected first, followed by the hands and arms.
Peripheral neuropathy can affect one, two, or all three of your nerves. Mononeuropathy is a condition in which only one nerve is affected.
Motor neuropathy symptoms include:
- muscle cramps
- twitching
- muscle weakness
- foot drop
- muscle wasting
- paralysis
Peripheral neuropathy causes a variety of symptoms, some more symptoms are-
- Numbness or reduced ability to feel pain or temperature changes
- Tingling or burning sensation
- Sharp pains or cramps
- Increased sensitivity to touch — for some people, even a bedsheet’s weight can be painful
- Serious foot problems, such as ulcers, infections, and bone and joint pain
Charcot’s foot
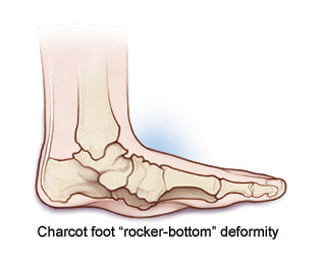
Charcot’s disease is a rare but dangerous complication that can affect those with peripheral neuropathy, particularly those with diabetes mellitus. Charcot affects the bones, joints, and soft tissues of the foot or ankle.
Bone fractures and sprains can occur. The bones become weak, and they may break, as well as the foot or ankle joints dislocating. If a fracture is not treated in its earliest stage, the joints in the foot will collapse, resulting in a deformed foot.
Pressure sores can develop in a foot or ankle with a deformed foot. An infection and possibly limb removal may occur as a result of an open wound with foot malformation.
Who gets Charcot’s Foot
Charcot’s foot is most commonly seen in diabetic patients, but it can also be caused by other factors. These include injuries to the nerves or blood vessels of the lower legs and untreated high blood pressure which results in poor circulation.
The condition mostly affects people who have had diabetes for a while (typically over 25 years), although it can occur earlier.
Symptoms of Charcot’s Foot
The foot is red, warm to the touch, and severely swollen in the early phases.
Causes of Charcot’s Foot
People who can’t feel anything in their feet and ankles because of nerve damage are susceptible to Charcot’s foot. Diabetes is a typical issue for individuals with this condition. Nerve damage may be caused by a variety of factors, however:
- Alcohol or drug abuse
- An infection
- Spinal cord disease or injury
- Parkinson’s disease
- HIV
- Syphilis
There is no known cause for Charcot’s foot. However, some factors can aggravate it:
- A sprain or broken bone that doesn’t get treatment quickly
- A sore on your foot that doesn’t heal
- An infection
- Foot surgery that heals slowly
Complications of Charcot Foot
Your bones might break and move out of place as they become weaker. When this happens:
- Your foot may lose its shape. The arch in your foot may fall until the bones are lower than your heel or toes. This is known as “rocker bottom” by doctors.
- Your toes may curl.
- Your ankle might become twisted and unsteady.
- Bones may press against your shoes. It’s important to keep your diabetic foot properly moisturized. Sores can develop on your skin as a result of not doing so.
- Your circulation may be restricted, which makes it more difficult for infections to heal. If this persists for an extended period of time, you may require amputation of your foot.
Diabetic Foot Pain Ulcers

Diabetic foot ulcers are one of the most common diabetic complications. In fact, they can affect up to 30% of people living with diabetes. As a result of nerve damage from diabetic neuropathy, it is difficult for your body to heal itself and recuperate after an injury.
This means that wounds have a tendency to linger. If diabetic ulcers are left untreated, they can become severe and even lead to amputation.
Foot ulcers are most prevalent under your big toes and ball of the feet, affecting your feet all the way down to the bones. All persons with diabetes can develop foot ulcers, although good foot care may help avoid them. The treatment for diabetic foot ulcers is determined by their origins.
Symptoms of Foot Ulcer
The black tissue (eschar) surrounding a severe foot ulcer is the most visible symptom. This occurs as a result of an absence of adequate blood flow to the surrounding area.
The ulcer can cause gangrene, which refers to tissue death as a result of infections. In this situation, there might be a noxious odor, discomfort, and numbness.
Foot ulcers are difficult to detect. You may not exhibit symptoms of the ulcer until it has become infected, despite the fact that you have a painful ulcer.
If you notice any skin discoloration, especially tissue that has turned black, or feel any discomfort in an area that appears callused or irritated, talk with your doctor.
Your doctor will most likely assess your ulcer’s severity using the Wagner Ulcer Classification System, which ranges from 0 to 5.
- 0: no open lesions; may have healed lesion
- 1: superficial ulcer without penetration to deeper layers
- 2: deeper ulcer, reaching tendon, bone, or joint capsule
- 3: deeper tissues involved, with abscess, osteomyelitis, or tendonitis
- 4: gangrene in a portion of forefoot or heel
- 5: extensive gangrenous involvement of the entire foot
Causes of Foot Ulcers
Ulcers in people with diabetes are most common by:
- poor circulation
- high blood sugar (hyperglycemia)
- nerve damage
- irritated or wounded feet
Poor blood circulation is a form of vascular disease in which blood does not flow to your feet adequately. Poor circulation can also make ulcers more difficult to heal.
Blood sugar management is important for healing a foot ulcer because high glucose levels can impede the advancement of wound healing. People with type 2 diabetes and other illnesses have a harder time fighting off infections from ulcers, according to studies.
Nerve damage is a long-term consequence that can result in a loss of feeling in your feet. Damaged nerves can feel tingly and painful. Nerve damage reduces sensitivity to foot discomfort, resulting in painless wounds that might develop ulcers.
Ulcers are by the presence of drainage from the afflicted region and, in some cases, a visible lump that isn’t always painful.
Diabetic Sores on Leg

Diabetes sores are open wounds that diabetic people get on their legs. Diabetic sores occur when the diabetic person does not have enough blood flow to heal a wound site, which can happen because of nerve damage in diabetics or because they do not check themselves often for cuts and scrapes. These foot ulcers are one of the most common diabetic complications.
The sores need to be in treatment right away because they can lead to infections. This can cause gangrene and ultimately amputation if not caught early enough. Diabetic sores should be cleaned with soap and water as soon as you notice them on your diabetic leg.
Diabetic sores should be treated with antibiotic ointment, bandaged, and elevated to prevent infection. The sores that are not properly cared for can lead to the loss of a limb or even death in severe cases if they get infected.
These foot ulcers are one of the most common diabetic complications because diabetics do not take care of diabetic sores in their legs.
Causes of Diabetic Sores
Diabetic sores are caused by the diabetic person not checking themselves often for cuts and scrapes, or diabetes-related nerve damage. Diabetics may also develop diabetic foot ulcers because of high blood sugar levels, which can destroy blood vessels in their legs.
Diabetics have a higher risk of infection too because they have less sensation in diabetic sores so they may not notice or feel a diabetic sore on their leg.
When to See a Doctor
Anyone who has diabetes should visit a doctor on a regular basis as part of their treatment. If any of the following changes are present, you should seek immediate medical attention:
- changes in skin color on the foot
- swelling in the foot or ankle
- temperature changes in the feet
- persistent sores on the feet
- pain or tingling in the feet or ankles
- ingrowing toenails
- athlete’s foot or other fungal infections of the feet
- dry, cracked skin on the heels
- signs of infection
Treatment of Diabetic Foot Pain
Treatment for diabetic foot problems varies according to the severity of the condition. Surgical and nonsurgical treatments are available in a variety of forms.
Nonsurgical Treatment
A doctor will first try to address diabetic foot issues without resorting to surgery. Some approaches include:
- keeping wounds clean and dressed
- wearing immobilization devices, such as a cast boot or total contact cast
- closely observing any gangrene on the toes until self-amputation occurs, which is when the toes fall off due to lack of blood flow
Surgical Treatment
If non-surgical treatment fails to cure diabetic foot issues, the doctor may advise surgery. The following are some of the surgical treatments available:
- the removal of decaying or dead tissue
- amputation, ranging from single toes or sections of the foot to amputation of the leg below or even above the knee
- surgical stabilization of Charcot’s Foot
- an arterial bypass for peripheral vascular disease, which assists blood flow to the area
- endovascular surgery with placement of stents, which uses small devices to keep blood vessels open.
Diabetic Foot Pain Care

This is so important. Diabetic foot pain can occur in the feet and lower limbs of diabetic patients, resulting from damage to nerves and blood vessels caused by diabetes mellitus.
- Check the feet every day: Check them for any changes or injuries, or have someone check them for you.
- Daily washing of the feet is in recommendation: to avoid infections, keep the feet clean.
- Protect your feet with socks and shoes at all times. At all times, wear socks and boots that protect the feet.
- To assist prevent deformities, a podiatrist may advise you to use special shoes. Do not wrap your toes in socks so tightly that blood flow is in restriction.
- Put the feet up when sitting, wiggle the toes from time to time, and get enough exercise to keep blood flowing to your feet. These methods assist in promoting optimum blood flow to your feet.
- Trim your nails carefully: Toenails should be trimmed straight across and kept short. Nail infection can develop as a result of rounded nails growing inward.
- Treat corn and bunion care with special attention. Shave corns only if absolutely necessary because this raises the risk of infection.
- Keep your feet safe from extreme temperatures: Diabetes-linked foot damage can be by excessive heat and cold.
- Checkups for the feet must be conducted on a regular basis: Regular check-ups by a doctor are essential for preventing infections, amputations, and significant deformities.
- Reduce blood sugar levels: Uncontrolled blood sugars put diabetic podiatric problems on steroids.
- Smoking increases the risk of foot problems in people with diabetes. Smoking depletes blood flow to the tissues, which can make diabetic foot issues worse.
Diabetic Foot Pain Prevention
Diabetic neuropathy is a problem that affects the nerves in the feet and legs, causing severe discomfort and pain. It’s also possible to prevent or reduce many of these problems by managing diabetes.
The best method to avoid these serious problems is to follow the advised diabetes treatment plans, but self-care and frequent checkups with a doctor can also assist prevent issues from occurring.
Conclusion
This blog post provides information about diabetic foot pain. It is imperative that you know the signs of this condition so you can get treatment right away to avoid serious complications and injury. The first step in treating your diabetes-related foot problems is making sure there are no ulcers or infections on the feet, which can be a sign of infection or cellulitis. If it does not clear up after one week with antibiotics, see a podiatrist for further diagnosis and treatment options such as surgery if necessary. You should also make sure that any calluses or corns do not become infected, because they may need surgical removal to prevent future infection from spreading into other parts of the body like bones and joints.
Do you want to get rid of diabetes? Join our online diabetes consultation program and reverse your Diabetes naturally through lifestyle changes such as a Personalized Diet plan, Exercise, dieticians, and health coaches.