Contents
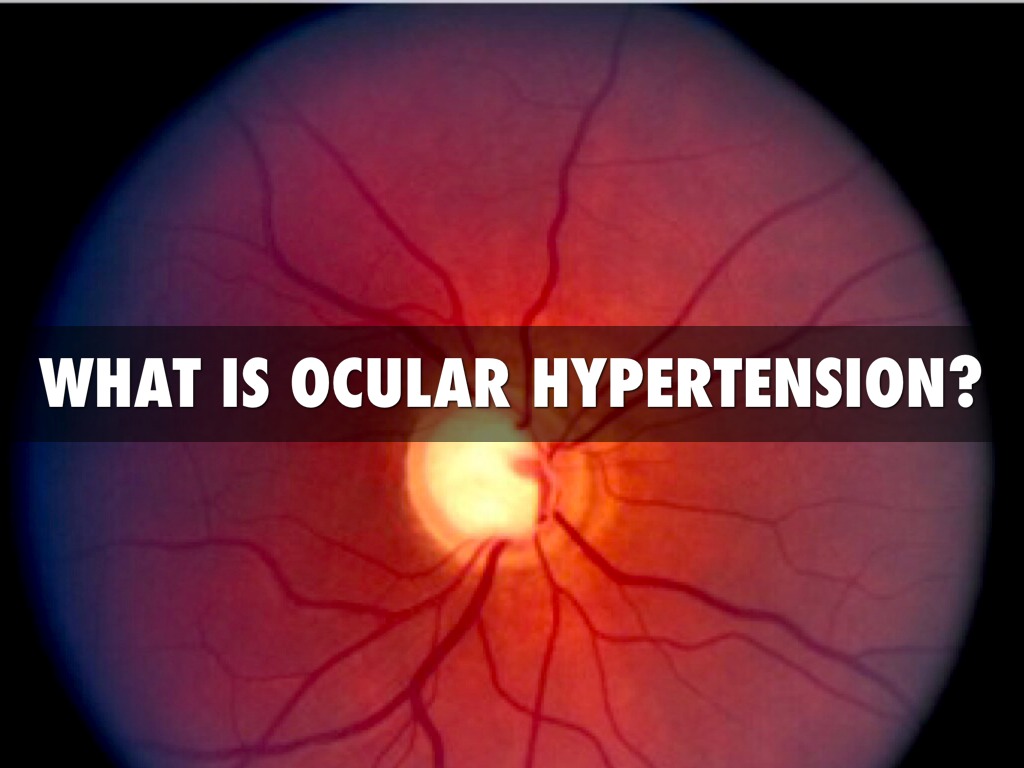
Ocular Hypertension
Ocular hypertension refers to the pressure in your eyes or your intraocular pressure (IOP). It is higher than normal. High eye pressure, if left untreated, can lead to glaucoma and permanent visual loss in certain people. Ocular hypertension can affect some people without causing vision or eye impairment, as assessed by a full eye exam and visual field tests.
Researchers have discovered that high eye pressure affects up to 9.4% of adults aged 40 and high. It is 10 to 15 times more common than primary open-angle glaucoma. However, the most common type of glaucoma.
According to research findings, around 10% of patients with untreated ocular hypertension develop primary open-angle glaucoma within five years. As a result, these individuals should have their ocular pressure checked regularly to avoid acquiring glaucoma.
Ocular Hypertension v/s Glaucoma
When the pressure inside the eye (intraocular pressure, or IOP) is higher than usual, it is known as ocular hypertension. The term “ocular hypertension” refers to an increase in the pressure of the fluid inside the eye. Glaucoma is more likely to occur in people who have ocular hypertension.
Eye pressure is sometimes called intraocular pressure (IOP). It is measured using a tonometry instrument. The measurement of pressure is in millimetres of mercury (mmHg). The normal range for ocular pressure is 10 to 20 mmHg.
Ocular hypertension is an increase in ocular pressure of more than 20 mmHg for two consecutive days without the presence of glaucoma alterations.
There are usually no indications or symptoms of ocular hypertension. Because high eye pressure puts you at a higher risk for glaucoma. It’s important to see your ophthalmologist for frequent eye exams.
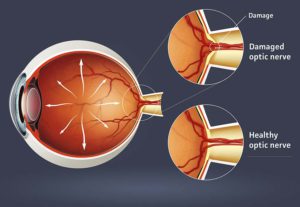
The optic nerve is more than 1 million nerve fibres. It makes up the visual nerve. However, it is the link between the retina and the brain.
Glaucoma is a collection of diseases that affect the optic nerve of the eye, which can lead to vision loss and blindness. Early detection and treatment, on the other hand, can often prevent your eyes from catastrophic vision loss.
Glaucoma is the most common cause of blindness in persons over the age of 40. Glaucoma-related blindness, on the other hand, can generally be avoided with early treatment.
Causes of Ocular Hypertension
A transparent fluid termed aqueous tumour is constantly produced by the eye. This enters the front part of the eye to provide nutrition. To maintain normal ocular pressure, an equal amount of fluid flows out at the same time. When this drainage mechanism fails, fluid builds up in the eye and intraocular pressure rises. This resulting in ocular hypertension.
Factors that induce or are linked to ocular hypertension are similar to those that cause glaucoma. These are some of them:
Excessive Aqueous Production
The aqueous is a transparent fluid produced inside the eye by the structure body. It is located behind the iris. The aqueous fills the anterior chamber of the eye after passing through the pupil (the space between the iris and the cornea).
The aqueous drains from the eye through the trabecular meshwork. It is located near the cornea and iris on the periphery of the anterior chamber. The pressure in the eye rises when the ciliary body generates too much aqueous. This resulting in ocular hypertension.
Inadequate Aqueous Drainage
When aqueous drains slowly from the eye, the normal balance of aqueous production and drainage is disrupted. This resulting in high ocular pressure. In some people, certain drugs might cause this as a side effect.
Steroid medications, for example, have been demonstrated to raise the risk of ocular hypertension. It happens when used to treat asthma and other disorders. Ask your eye doctor how often you should have your IOP checked if you’ve been on steroid drugs for any reason.
Eye Trauma
Ocular hypertension can result from an injury to the eye. It disrupts the equilibrium of aqueous production and drainage. This might happen for few months or even years after the injury. Make sure to tell your doctor if you’ve had any eye injuries recently or in the past during your routine eye checkups.
Other Eye Conditions
Pseudoexfoliation syndrome, pigment dispersion syndrome, and corneal arcus are all diseases that have been linked to ocular hypertension. If you have any of these diseases, your eye doctor may advise you to undergo more frequent eye exams. Also, some measurements of your eye pressure will be noted.
Ocular hypertension and glaucoma risk are also affected by race, age, and family history. Though anybody can acquire high eye pressure. Those over the age of 40, and those who have a family history of ocular hypertension or glaucoma are at a higher risk.
According to some studies, people with thinner-than-normal central corneal thickness measurements are more likely to develop ocular hypertension and glaucoma.
Symptoms of Ocular Hypertension
 There are no external signs of ocular hypertension, as seen in eye pain or red eyes. So you can’t determine if you have it. It can only be detected by an ophthalmologist. Your eye doctor will test your IOP. They will compare it to normal levels during a full eye checkup. Ocular hypertension is defined as a reading of 21 mmHg (millimetres of mercury) or higher in the eye.
There are no external signs of ocular hypertension, as seen in eye pain or red eyes. So you can’t determine if you have it. It can only be detected by an ophthalmologist. Your eye doctor will test your IOP. They will compare it to normal levels during a full eye checkup. Ocular hypertension is defined as a reading of 21 mmHg (millimetres of mercury) or higher in the eye.
Ocular Hypertension Risk Factors
The chance of having ocular hypertension is increased by a variety of factors. It does not affect everyone who has risk factors. The following are some of the risk factors:
- Hispanic heritage
- Having diabetes or high blood pressure
- Eye injuries or surgeries
- Family history of ocular hypertension
- Age 40 years or older
- Use of corticosteroid medicines for a long time
Diagnosis of Ocular Hypertension
Many of the factors that led to ocular hypertension are out of your control. Your genetics are unchangeable. However, if you have medical problems that enhance your risk, then you can follow steps to reduce the risk factors. It can be avoided by managing your blood sugar, blood pressure, and other eye diseases.
- It’s important to follow eye care instructions regularly. Doctors use a tonometer to assess intraocular pressure during a comprehensive eye checkup.
- This utility is available in several distinct versions. A frequent method is to use a puff of air to flatten the cornea for a short period. The amount of flattening indicates the pressure inside your eye to your doctor.
- In your 20s, you should get a baseline eye exam, and in your 30s, you should see your eye doctor twice. You should undergo a comprehensive eye exam once you reach the age of 40.
- Your doctor will use the results to determine how often you should return. These recommendations may alter if you have a family history of ocular hypertension or glaucoma. Consult your eye doctor to determine how frequently you should undergo checkups.
You can better comprehend why ocular hypertension should be maintained. Only if you imagine your eye as a globe inflated by pressure. When your eye pressure is too high or continues to rise, it exerts a force on the sensitive optic nerve inside your eye, resulting in glaucoma.
Consult your eye doctor frequently if you have any risk factors for ocular hypertension. A full eye exam with tonometry is the only way to find out excessive intraocular pressure.
Ocular Hypertension Treatments
If your eye doctor determines you with ocular hypertension, he or she may prescribe eye drops to lower your eye pressure. Because these treatments might create negative effects. Some eye doctors prefer to keep an eye on your IOP. However, intervene only if you show additional signs of glaucoma.

Your eye doctor may offer alternative glaucoma treatment procedures. Such as glaucoma surgery, to relieve excessive eye pressure in some circumstances (or if eye drops are ineffective in lowering your IOP). Because of the increased risk of glaucoma with ocular hypertension, you should get your IOP checked regularly to keep track of your condition.
Your ophthalmologist may determine that you require eye-drop medication. It is to reduce your intraocular pressure. Within a few weeks of starting the prescription, they will schedule a visit to see how it is working.
Your ophthalmologist may prescribe more than one medication in some cases. For the drops to function, you must follow the instructions given. To lower eye pressure, a laser or surgery may be utilized. Treatment reduces your glaucoma risk, but it does not eradicate it. Glaucoma can develop in certain people who have ocular hypertension.
Medication For Ocular Hypertension
The ideal medicine for treating ocular hypertension would effectively lower IOP. It will have no side effects or systemic worsening of the disease. Hence, affordable, and have once-a-day dosing. Because no medicine currently possesses all of the criteria listed above.
These characteristics should be prioritized. It is based on the patient’s individual needs and risks. Therefore, therapy should be chosen appropriately.
In the treatment of this, older glaucoma drugs such as cholinergic (i.e., miotics, such as pilocarpine), osmotic, and nonselective adrenergic agonists have limited use. Only if contraindications impede the use of preferred medications that are needed to be considered.
Home Remedies For Ocular Hypertension
Your ophthalmologist prescribes medicines to help in lowering the pressure inside your eye. It’s important to follow your doctor’s instructions. Also, follow the medication correctly. Failure to do so may increase intraocular pressure. This is resulting in optic nerve injury and permanent vision loss.
These suggestions may help in the management of high eye pressure or the wellness of eye health:
- Eat a healthy diet: A nutritious diet can help you stay healthy. But it won’t stop your glaucoma from getting worse. Zinc, copper, selenium, and the antioxidant vitamins C, E, and A are all vital for eye health.
- Exercise safely: Regular exercise may help to lower ocular pressure. Consult your doctor about an exercise regimen that is right for you.
- Limit your caffeine: caffeine-rich beverages may cause an increase in your blood pressure.
- Sip fluids frequently: At any one point during the day, only drink moderate amounts of fluids. Drinking a quart or more in a short period of time can cause temporary ocular pressure to rise.
- Sleep with your head elevated: It’s been proven that sleeping with a wedge pillow will keep your head slightly lifted. It is roughly 20 degrees, lowers intraocular pressure.
- Take prescribed medicine: Taking your eyedrops or other medicines exactly as prescribed can help you obtain the best results from your treatment. Make sure you’re using the drops exactly as prescribed. Otherwise, the damage to your optic nerve may worsen.
A Word From Mantra Care
If you are looking for an affordable hypertension treatment MantraCare can help- Book a trial hypertension care session