Contents
Skin Conditions and Diabetes
can affect many parts of your body, including your skin. When diabetes affects the skin it’s often a sign that your blood sugar levels are too high. If you have skin conditions in diabetes, it could mean-
- You have undiagnosed diabetes or pre-diabetes
- Your treatment for diabetes needs to be adjusted
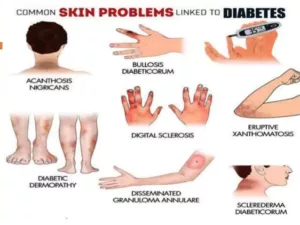
Skin Conditions Linked To Diabetes
Skin conditions related to diabetes are common. As many as 1 out of 3 people with diabetes will have one. Fortunately, most skin conditions can be successfully treated before they turn into a serious problem. The key is to catch them early. Early diagnosis helps in early treatment.
Before discussing each condition in detail, let me tell you some more common skin problems like itchy skin and bacterial & fungal infections that a person with diabetes may experience-
Itchy skin

Itching skin, also called pruritus, can have many causes, such as dry skin, poor blood flow, or a yeast infection. When itching is caused by poor blood flow, you’ll likely feel it in your lower legs and feet. Lotion can help to keep your skin soft and moist and prevent itching due to dry skin.
Bacterial Infection
 Staphylococcus skin infections are more common and more serious in people with poorly controlled diabetes. When hair follicles are irritated, these bacteria can cause boils or an inflamed bump. Other infections include:
Staphylococcus skin infections are more common and more serious in people with poorly controlled diabetes. When hair follicles are irritated, these bacteria can cause boils or an inflamed bump. Other infections include:
- Styes, which are infections of the eyelid glands
- Nail infections
Most bacterial infections need to be treated with antibiotic pills. Talk with your doctor for effective treatment.
Fungal infections

Warm, moist folds of the skin are the perfect breeding ground for these infections.
Three common fungal infections are:
- Jock itch (red, itchy area on the genitals and the inside of the thighs)
- Athlete’s foot (affects the skin between the toes)
- Ringworm (ring-shaped, scaly patches that can itch or blister and appear on the feet, groin, chest, stomach, scalp, or nails).
Now let’s talk about the skin conditions that diabetes may bring. Common conditions are-
Acanthosis nigricans
 This condition is most common in people with type 2 diabetes. It causes darkened and thickened skin, especially in skin folds. It looks like a small wart. Skin becomes tan or brown. It’s sometimes slightly raised and may look velvety. It can be found on the sides or back of the neck, the armpits, under the breast, and groin. Sometimes, the top of your knuckles will look strange. This condition usually affects people who are very overweight. It usually starts before diabetes, and it can be a sign of insulin resistance. While there’s no cure, losing weight may help.
This condition is most common in people with type 2 diabetes. It causes darkened and thickened skin, especially in skin folds. It looks like a small wart. Skin becomes tan or brown. It’s sometimes slightly raised and may look velvety. It can be found on the sides or back of the neck, the armpits, under the breast, and groin. Sometimes, the top of your knuckles will look strange. This condition usually affects people who are very overweight. It usually starts before diabetes, and it can be a sign of insulin resistance. While there’s no cure, losing weight may help.
Diabetic Dermopathy
This condition happens due to changes to the blood vessels in your skin. Dermopathy appears as a shiny round or oval lesion on the thin skin of your shins. The patches don’t hurt, and they rarely cause itching or burning. Treatment usually isn’t necessary.
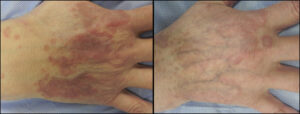
Necrobiosis Lipoidica Diabeticorum
If you’ve had diabetes for a long time without good control of your blood sugar, you could develop this condition. Poor blood supply to the skin can cause changes in the collagen and fat underneath. The overlying skin becomes thin and red. Most lesions are found on the lower parts of the legs and can turn into an ulcer if there’s trauma. Lesions have fairly well-defined borders. Sometimes, the condition is itchy and painful. As long as the sores don’t break open, you won’t need treatment for them. If the sores do break open, see your doctor.
Digital Sclerosis
Due to poor blood flow, the skin on your toes, fingers, and hands becomes thick, waxy, and tight. It can also make your finger joints stiff. Get your blood sugar under control, because that can help treat this condition. Try lotions and moisturizers to help soften the skin.
Eruptive Xanthomatosis
 Severe insulin resistance can make it hard for your body to get rid of fat in your blood. When you have very high cholesterol, this skin condition can happen. Firm, yellow, waxy pea-like bumps on the skin are surrounded by red halos and are itchy. These usually show up on the eyes, elbows, face, and buttocks. They also can appear on the backside of the arms and legs. To treat it, your doctor will work to control the level of fats in your blood. The bumps usually go away over several weeks.
Severe insulin resistance can make it hard for your body to get rid of fat in your blood. When you have very high cholesterol, this skin condition can happen. Firm, yellow, waxy pea-like bumps on the skin are surrounded by red halos and are itchy. These usually show up on the eyes, elbows, face, and buttocks. They also can appear on the backside of the arms and legs. To treat it, your doctor will work to control the level of fats in your blood. The bumps usually go away over several weeks.
Bullosis Diabeticorum
In rare cases, people with diabetes get blisters that resemble burn blisters. These can affect the fingers, hands, toes, feet, legs, or forearms. They’re usually painless and they heal on their own. They often happen in people who have severe diabetes and diabetic neuropathy. For treatment, your doctor will help you get your blood sugar levels under control.
Disseminated Granuloma Annulare
While there is some controversy over whether this condition is connected to diabetes, disseminated granuloma annulare causes sharply defined ring- or arc-shaped areas on the skin. These rashes most often happen on the fingers and ears, but they can appear on the chest and abdomen, too. The rash can be red, red-brown, or skin-colored. Treatment usually isn’t needed, but sometimes a steroid medication you put on your skin can help.
Scleredema Diabeticorum
This condition causes a thickening of the skin on the back of the neck and upper back. It’s rare, but it can affect people with type 2 diabetes. The treatment is to bring your blood sugar levels under control. Lotions and moisturizers might help soften your skin.
After understanding each skin problem or condition that people with diabetes may experience. Let’s talk about how one can prevent them-
Preventions Of Skin Conditions In Diabetes

Keeping your diabetes under control is the most important factor in preventing Proper skincare and can also help reduce your risk of skin-related problems.
If you have diabetes, there are some steps you can take to help prevent skin problems. Consider the following tips for good skincare:
Keep your diabetes under control
Follow your healthcare provider’s advice about nutrition, exercise, and medication. Keep your blood glucose level within the range recommended by your healthcare provider.
Skincare
Keep your skin clean and dry, while bathing or showering, use warm water and mild, moisture-containing soap. After washing, make sure to rinse and dry yourself well (pat your skin dry; do not rub). Check places where water can collect, such as under the arms, under the breasts, between the legs, and between the toes. these are the other skincare routine you can follow-
- Look at your body after you wash. Make sure you don’t have any dry, red, or sore spots that could become infected.
- Avoid bathing in hot water and taking long baths or showers. Also avoid bubble baths, which often contain detergents that can be drying. Avoid scratching dry skin. Apply moisturizer instead.
- Keep your skin moist by using a lotion or cream after you wash. Ask your healthcare provider to suggest a good lotion. Keep a bottle of lotion near the sink so you can use it after washing your hands. You should use a fragrance-free and dye-free moisturizer.
- Apply lip balm to prevent chapped lips.
- Limit the products you use on your skin to decrease your chances of having a reaction.
- Treat cuts right away. Wash them with soap and water. Avoid antiseptics, iodine, or alcohol to clean cuts, because they are too harsh. Ask your healthcare provider to recommend an antibiotic cream or ointment to use on minor cuts.
- Drink lots of fluids, especially water, to keep your skin moist and healthy.
- To prevent dry skin when the temperature drops, use a room humidifier to add moisture to heated, indoor air.
- To protect your skin from the sun, use sunscreens with an SPF of 30 or higher on your nose, and wear a hat. In colder months, wear warm gloves and shoes or boots.
- Wear all-cotton white underwear. Cotton allows air to move around your body.
Tips for Skin Conditions Care In Diabetes

If you have any skin problems, first of all, consult with a doctor. After that you can prepare a first aid kit at home, to make sure that you take care of them whenever needed.
You can keep a first-aid kit handy to take care of your hands and feet. It should contain- antibacterial ointment, gauze pads, hypoallergenic tape or paper tape, and prepackaged cleansing towelettes in case you are out or soap and water are not available.
If you have any blisters, don’t break or pop them. Gently wash the area with a bar of mild soap and warm water and apply an antibacterial ointment. Follow the same process in case of any small cuts, skin irritation, or minor burns. You can also cover them with a gauze pad and secure them with paper tape. If you do so make sure to change the bandage every day.
When To Call A Doctor?
You should call the doctor if you’re feeling itchy anywhere and the condition is not getting any better the day after treating the problem. If the pain or discomfort continues for more than two days or you develop a fever. If you notice any pus developing in any part of your body.
Also if you notice any change in your skin, you should mention that to your doctor for sure.
A Word From MantraCare
Do you want to get rid of diabetes? Join our online diabetes consultation program and reverse your Diabetes naturally through lifestyle changes such as a Personalized Diet plan, Exercise, dieticians, and health coaches.


