Contents
What Is Charcot Foot?
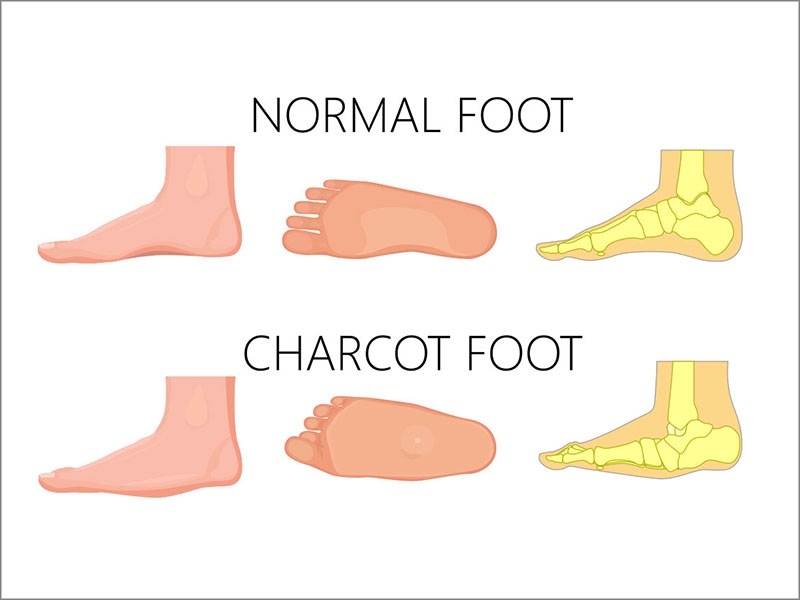
Charcot’s foot is a rare but deadly condition that can occur in people with peripheral neuropathy, particularly in those who have diabetes. The bones, joints, and soft tissues of the foot and ankle are all affected by Charcot. The bones of the foot or ankle grow weak and can shatter, and the joints can dislocate.
The joints of the foot collapse if not caught early on, and the foot finally becomes deformed. Pressure sores in the foot or ankle can occur as a result of a deformed foot. An infection or amputation might result from an open wound with a foot deformation.
Pain from fractures or other traumas can go unrecognized because the foot is numb, resulting in extra injury from walking and standing. The joints of the foot might dislocate or collapse as the bones deteriorate, affecting the form of the foot. The resulting shape is known as a rocker-bottom foot because the arch extends down and out, resembling a rocker.
Charcot foot can also cause painful sores that are difficult to heal. Charcot foot can result in severe deformity, disability, or amputation if left untreated.
Symptoms of Charcot Foot
- Swelling in foot or ankle
- Redness in foot or ankle
- Warm feeling in the point of injury
- A deep aching feeling
- Deformation of the foot
Neuropathy can develop and become much more serious as a result of diabetes, so people with diabetes should report any signs of a foot injury to their doctor as soon as possible. If not handled by a doctor or professional, more serious foot disorders can lead to amputation.
Causes of Charcot Foot
People with numbness in their feet and legs develop Charcot’s feet. Peripheral neuropathy is a type of nerve injury that causes a loss of sensation. Although Charcot’s foot is most closely associated with diabetes as an uncommon consequence. However, peripheral neuropathy is linked to a variety of illnesses.
Unrecognized sprains or injuries are a typical occurrence. Because the person suffering from peripheral neuropathy is unable to perceive pain or other feelings. The injury may go undiagnosed. If a broken bone in the foot or ankle is not treated properly, it might deteriorate, resulting in foot sores and infection.
In diabetic patients, Charcot’s foot has also been seen as a complication after organ transplantation. (This is due to the use of medicines to prevent organ rejection, which also causes bone loss and fractures as a side effect.) However, some of the other main causes of Charcot’s foot are:
- Diabetes
- Drug abuse
- Leprosy
- Alcohol use disorder
- Syphilis
- HIV
- Infection or trauma
- Damage to peripheral nerve
- Inflammatory conditions
- Polio
Stages of Charcot Foot
Charcot Foot usually occurs in three stages:
Fragmentation And Destruction
Symptoms such as redness and severe swelling of the foot and ankle characterize this acute stage. When compared to the other foot, the area may also seem warm or heated to the touch.
Soft tissue swelling and tiny bone fractures are beginning to appear on the inside. As a result, the joints and surrounding bone are damaged. However, the joints lose their rigidity and get dislocated. The bones may potentially jellify, entirely softening.
The bottom of the foot may take on a flat or rocker-bottomed appearance during this period. Plantar prominences are bony protrusions that can form on the bottom of the foot. This stage can persist for up to a year if not treated.
Coalescence
The body works to repair the harm caused by the first stage during coalescence. Swelling, redness, and warmth decrease the destruction of the joints and bones. It also makes the joints and bones function slow. The authors discovered that the hydrophilic emulsifier is primarily responsible for coalescence events.
Based on direct microscopic observations, the scientists were able to calculate the concentration of external emulsifiers that will cause the inner droplets to coalesce and the concentration of the inner surfactant that will cause the coalescence to begin in the router interfacial layer.
The coalescence principle’s effect is based on the movement of numerous droplets into a compact liquid phase (contaminant-oil phase). The development of huge surfaces produced by arranging plate packs or packing parts in a separate tank supports the coalescence principle.
Solids will attach to the surfaces due to their large surfaces, which is a disadvantage. The plate pack or packing elements must be removed and mechanically cleaned regularly, depending on the emulsion contamination.
Reconstruction
The foot’s joints and bones mend during this third and final stage. Unfortunately, they do not return to their previous state or shape on their own. While no additional harm gets to the foot, it is frequently left misshapen and unstable. The foot may also be more prone to sores and ulcers, which can lead to greater deformity, and, in some circumstances, there is a need for surgery.
Complications of Charcot Foot
The bone rubbing on the shoe or the ground can create skin ulcers in any part of the foot or ankle. Because tissue has replaced the bone in the joint when Charcot’s foot affects the ankle, the joint may become unstable or “floppy.” Ulcers can also be caused by the “floppy foot.”
Due to diabetes issues, poor circulation in the feet, being on your feet for long periods, and the development of infections, ulcers are often difficult to cure. A non-healing infected ulcer can be life-threatening and even result in amputation of the foot or leg.
Preventive Care For Charcot Foot
By taking the following steps, the patient can help prevent Charcot foot and its complications:
- Maintaining a healthy blood sugar level can help slow the progression of nerve damage in the foot.
- Have an appointment for your feet and ankles to be examined by a foot and ankle surgeon regularly.
- Check both feet every day, and if you find any signs of Charcot foot, visit a surgeon right away.
- Avoid injuries by not stumbling on your foot or overdoing an exercise routine.
- To avoid recurrences, ulcers, and amputation, follow the surgeon’s instructions for long-term care.
Diagnosis of Charcot Foot
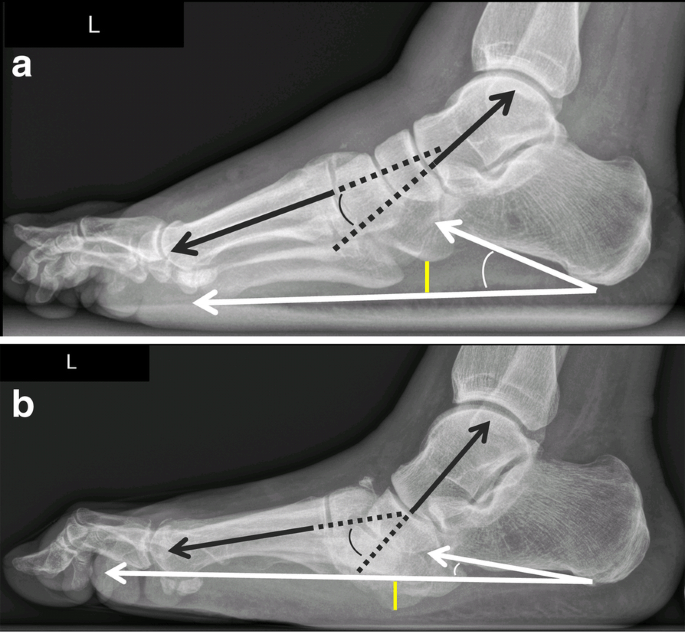
Because X-rays may not pick up on the damage that is beginning to occur during stage one, Charcot foot may go untreated. As a result, it’s important to inform your doctor if you have a medical condition that could lead to Charcot foot. Imaging tools such as X-rays and MRIs can be beneficial in the latter stages of cancer after it has progressed.
A physical exam, a review of your medical history, and testing will be used by your doctor to look for indicators of neuropathy in addition to examining your symptoms. These may include the following:
- Semmes-Weinstein Pinprick test, which examines the ability to feel.
- Pain neurometer test, which determines the peripheral nerve.
- Dysfunction 5.07/10-gram monofilament test, which analyses sensitivity to pressure and touch in major nerve fibers.
Your doctor will also examine the muscle tone and strength in your leg and foot, as well as test your tendon reflexes. Following are some of the ways by which your doctor will examine your charcot foot:
Medical History and Physical Examination

Your doctor will discuss your overall health as well as any symptoms you may be experiencing. If you know how you damaged your foot, your doctor will want to know about it as well.
Your doctor will check your foot after discussing your symptoms and medical history.
Magnetic Resonance Imaging (MRI) and Ultrasound
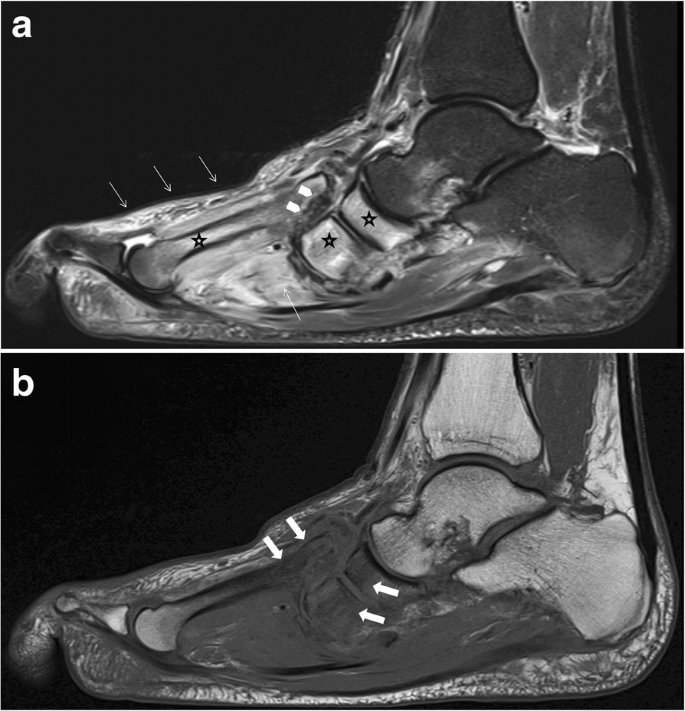
In MRI, researches may help to improve imaging of the soft tissues of the foot and ankle. If your doctor detects a bone infection, this may be prescribed. Infection of the bone is extremely rare if there is no rapture in the skin.
However, Magnetic Resonance Imaging is a radiological imaging technology that creates images of the anatomy and physiological processes of the body. Strong magnetic fields, magnetic field gradients, and radio waves are used in MRI scanners to create images of the body’s organs. This process is used to examine the Charcot foot problem of the patient.
Bone Scan/Indium Scan
A bone scan is a nuclear medicine test that can be used to determine whether or not a patient has a bone infection. Different types of bone scans exist, and the doctor must evaluate which type(s) is best for a certain situation.
An indium scan is a specialist diagnostic that includes labeling white blood cells with a marker. These cells are followed to see if they are heading to the bone to fight.
Treatment for Charcot Foot
Early detection and treatment can help to prevent further injury, deformity, and other consequences. The treatment aims to relieve pressure on the foot, cure bone disease (typically with a cast, but bisphosphonates and other supplements may be used), and prevent new foot fractures.
Non-Surgical Treatment for Charcot Foot
Rest or removing weight from the injured foot (also known as “offloading”) is the first and most important treatment. Offloading is beneficial in the early stages of Charcot foot because it reduces inflammation, keeps the condition from worsening, and prevents deformity.
Later on, protected weight-bearing (walking in a walking boot) can help avoid consequences from the current deformity and additional deformities.
Offloading may entail placing the foot in a cast, which protects and immobilizes it. Over 8 to 12 weeks, the patient usually wears a series of casts or a detachable cast walker. To avoid putting any weight on the injured foot, can use crutches, a knee walker, or a wheelchair. As the swelling in the foot decreases, the cast is replaced multiple times. The foot will be in a cast until the redness, swelling, and heat have subsided.
After removing the cast, the doctor provides a prescription for footwear for the patient. Prescription orthopedic footwear fits the foot properly and reduces pressure points, reducing the risk of recurrent injury and ulceration. A Charcot Restraint Orthotic Walker (CROW) is a typical device use to avoid further foot injuries. The doctor may suggest that the patient’s activity needs to be changed.
Surgical Treatment For Charcot Foot

Patients with significant ankle and foot abnormalities that are unstable and at high risk of developing a foot ulcer should consider surgery.
Surgery may also be necessary if the abnormality renders braces and orthotics difficult to use. The patient will have to avoid putting full weight on the Charcot foot for a long time after surgery.
All people with Charcot foot must devote the remainder of their lives to wearing protective footwear and taking additional care of their feet. Preventing future problems begins with educating the patient and family members on proper foot care and warning signals to look for.
A Word From MantraCare
Do you want to get rid of diabetes? Join our online diabetes consultation program and reverse your Diabetes naturally through lifestyle changes such as a Personalized Diet plan, Exercise, dieticians, and health coaches.