Contents
- 1 Diabetic Retinopathy
- 2 Types of Diabetic Retinopathy
- 3 Symptoms of Diabetic Retinopathy
- 4 Causes of Diabetic Retinopathy
- 5 Four Stages of Diabetic Retinopathy
- 6 Risk Factors For Diabetic Retinopathy
- 7 Complications of Diabetic Retinopathy
- 8 Diagnosis of Diabetic Retinopathy
- 9 Treatment For Diabetic Retinopathy
- 10 Preventions of Diabetic Retinopathy
- 11 When To See An Eye Doctor
- 12 A Word From MantraCare
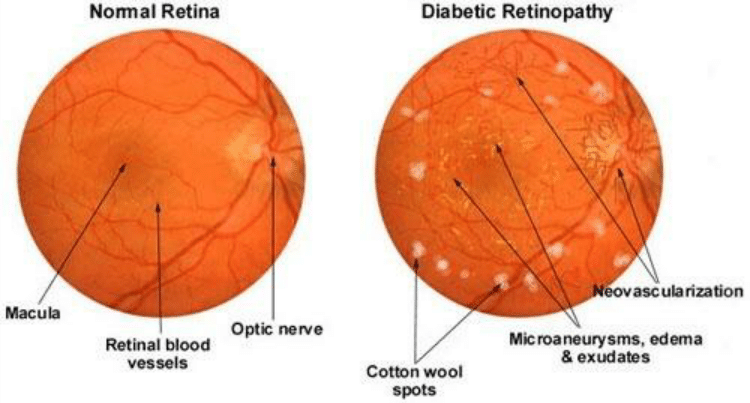
Diabetic Retinopathy
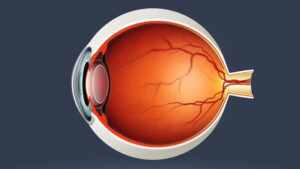
Diabetic retinopathy is an eye disease caused by diabetes. It causes damage to the blood vessels of the light-sensitive tissue in the rear of the eye (retina). Diabetic retinopathy may cause no symptoms or just minor vision problems at first. However, it may cause blindness. Anyone with type 1 diabetes or type 2 diabetes can develop the illness. This eye issue is more likely to develop the longer you have diabetes. Moreover, there is a chance for the patient to develop when your blood sugar is controlled.
Types of Diabetic Retinopathy
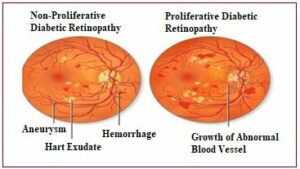
Nonproliferative Diabetic Retinopathy (NPDR)
The term “nonproliferative” refers to the fact that the eye does not produce new blood vessels in the early stages of diabetic retinopathy. Damaged blood vessels in the early stages of retinopathy frequently leak blood and fluid into the eye. The macula, or center of the retina, might swell in some situations.
This results in a condition known as macular edema. Mild, moderate, and severe NPDR are the three phases of the disease. Moreover, it might proceed to the other kind, or fourth stage, proliferative diabetic retinopathy.
Proliferative Diabetic Retinopathy (PDR)
The stage of retinopathy in which new blood vessels begin to develop within the retina is known as proliferative diabetic retinopathy. People also call it advanced retinopathy. These abnormal new blood vessels generally develop in the middle of the eye.
The retina might eventually detach from the back of your eye due to scar tissue formed by the development of new blood vessels. To note the relevant information, if the new blood vessels obstruct the usual flow of fluid out of the eye, pressure in the eyeball might build up. Also, glaucoma is caused by a build-up of fluid on the nerve that transmits pictures from your eye to your brain (optic nerve).
Symptoms of Diabetic Retinopathy
In the early stages of diabetic retinopathy, you may not notice any symptoms. As the illness worsens, you may experience:
- Blurred vision
- Vision loss
- Fluctuating vision
- Dark strings in vision
- Dark and empty areas in vision
Causes of Diabetic Retinopathy
Through the cutting off of the retina’s blood supply, too much sugar can induce a blockage in the small blood capillaries that nourish it. As a result, the eye makes an effort to form new blood vessels. However, these new blood vessels do not grow correctly and are prone to leakage.
Diabetes causes high blood sugar, which leads to diabetic retinopathy. Too much sugar in your blood can damage your retina, which detects light and sends signals to your brain through a nerve at the back of your eye (optic nerve).
However, diabetes damages blood vessels in the body which causes diabetic retinopathy. Sugar obstructs the tiny blood vessels that go to your retina. This is responsible for causing them to leak fluid or bleed, causing damage to your eyes. Your eyes start generating new blood vessels.
These blood vessels don’t operate adequately to compensate for the blocked blood vessels. These young blood vessels are prone to leaking or bleeding.
Four Stages of Diabetic Retinopathy
Patients with diabetes are at risk for neurovascular problems such as diabetic retinopathy and/or diabetic macular edema (DME). This is irrespective of whether they have type 1 or type 2. Diabetic retinopathy is a type of eye disease that affects people with diabetes. It occurs when excessive blood sugar destroys the retina’s tiny blood vessels.
This results in a wide range of symptoms, including blurred vision and vision loss. However, since this condition can cause irreversible vision loss, it’s necessary to get frequent eye checkups. Thus, you can diagnose the disease early and the progression will be controlled.
The two types are nonproliferative and proliferative. Nonproliferative refers to the early stages of the disease, while proliferative is an advanced form of the disease.
Mild Nonproliferative Diabetic Retinopathy
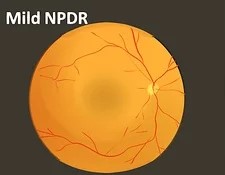
The first stage of diabetic retinopathy, which is characterized by tiny areas of swelling in the retina’s blood vessels. Micro aneurysms are the name for these swollen areas. At this point, small quantities of fluid might leak into the retina, causing macula swelling. This is an area of the retina near the center.
Moderate Nonproliferative Diabetic Retinopathy
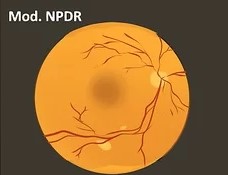
Swelling of tiny blood vessels begins to obstruct the blood supply to the retina, preventing appropriate nutrition. The macula becomes blocked with blood and other fluids as a result of this.
Severe Nonproliferative Diabetic Retinopathy
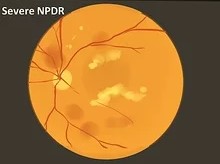
A greater part of the retina’s blood vessels becomes blocked, resulting in a substantial reduction in blood flow to this area. The body receives signals to begin developing new blood vessels in the retina at this stage.
Proliferative Diabetic Retinopathy
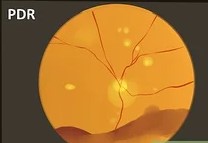
The disease has advanced to the point where new blood vessels are forming in the retina. Fluid leakage is much more since these blood vessels are typically weak.
This causes a variety of vision issues, including blurriness, a reduced field of vision, and even blindness.
Risk Factors For Diabetic Retinopathy
The risk of developing diabetic retinopathy can be high in people with diabetes. It can result in many conditions like an increase in:
- Pregnancy
- Excess use of tobacco
- High blood pressure
- High cholesterol
- Poor control of blood sugar level
- Having diabetes for a long time
Complications of Diabetic Retinopathy
Diabetics’ retinopathy can lead to serious complications. However, it involves the growth of abnormal blood vessels in the retina. These complications include:
Vitreous Hemorrhage
The new blood vessels may flow into the transparent, jelly-like material that fills your eye’s center. If the amount is insignificant, you may just see dark patches (floaters). Blood can fill the vitreous cavity and obscure your vision in more severe situations.
In most cases, a vitreous hemorrhage does not result in permanent visual loss. Within four weeks or months, the blood in the eye usually clears. Your eyesight will probably recover to its original sharpness unless your retina is injured.
Retinal Detachment
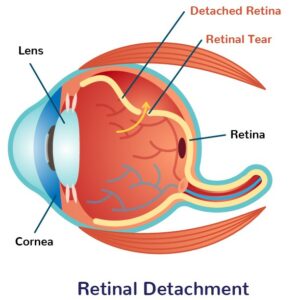
Diabetic retinopathy is connected with abnormal blood vessels that stimulate the development of scar tissue. It can pull the retina away from the rear of the eye. This can result in floating spots in your vision, bright flashes, or serious vision loss.
Glaucoma
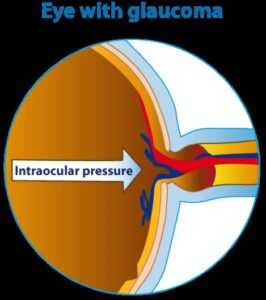
New blood vessels can form in the iris (front portion of the eye) and obstruct the usual flow of fluid out of the eye. It causes pressure to build up in the eye. The pressure might damage the nerve that transmits pictures from your eye to your brain.
Blindness
Diabetic retinopathy, macular edema, glaucoma, or a combination of these diseases can result in total vision loss. The patients are more prone if they are not treated properly.
Diagnosis of Diabetic Retinopathy
During your eye exam, your eye doctor can typically identify if you have diabetic retinopathy. However, the following can be considered as the diagnosis for diabetic retinopathy.
Pupil Dilation: Your doctor will dilate your pupils to check for any changes or new blood vessels in your eye. They’ll also check for bulging or detached retinas.
Fluorescein angiogram: If you have DME or severe diabetic retinopathy, this test can alert your doctor. It will reveal whether or not any of your blood vessels are leaking or damaged. Your doctor will give you a shot of fluorescent dye into a vein in your arm. Your doctor will be able to see images of the blood vessels in your retina. This will help him to detect any major problems once the dye reaches your eyes.
Treatment For Diabetic Retinopathy
Treatments will be determined with the disease’s stage and disease intensity. If detected early — before retinal damage develops — blood sugar control may be the sole therapeutic option. However, your doctor will continue to examine your eyes to ensure that the illness does not worsen.
If you’re at a nonproliferative stage but have some eye damage, you might try the following treatments:
- Laser surgery: It is a procedure that involves the use of Photocoagulation. It is a type of laser surgery, decreases the need for abnormal blood vessels and swelling in the retina.
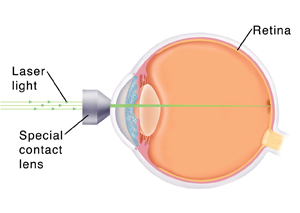
- Medications for the eyes: It is a steroid injection in the eye that can reduce inflammation and prevent new blood vessels from forming. Anti-VEGF medicine, which helps reduce swelling in the macula and enhance vision. It may potentially be a good option for you. Both therapies are given as an injection into the eye by doctors.

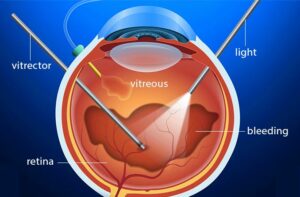
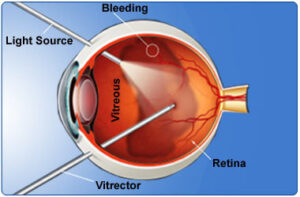
- Vitrectomy: If you have proliferative diabetic retinopathy, you may require vitrectomy surgery. The retina and vitreous, a jellylike material in the center of the eye, are treated with this surgery. Scar tissue, blood or fluid, and parts of the vitreous gel. It can be removed during surgery to allow light rays to focus properly on the retina. Traction in the retina or retinal detachments can be treated at the same time.
Preventions of Diabetic Retinopathy
Diabetic retinopathy is not always preventable. Regular eye checkups, excellent blood sugar, and blood pressure control, and early care for vision issues, can also help avoid serious vision loss.
However, diabetes retinopathy doesn’t always lead to vision loss. Therefore, it is necessary to manage your diabetes to prevent its complications.
Reduce the risk of diabetic retinopathy if you have diabetes through the following ways:
Manage Your Diabetes
- Make healthy food and exercise a regular part of your day.
- Each week, aim for at least 150 minutes of moderate aerobic activity, such as walking.
- Follow the directions on your diabetic medicine or insulin.
Monitor Your Blood Sugar Level
- You may need to check and record your blood sugar level many times a day — or even more often if you’re sick or stressed.
- Inquire with your doctor about how often you should test your blood sugar.
Know About Glycosylated Haemoglobin Test
- The glycosylated haemoglobin test measures your average blood sugar level over the previous two to three months. People often call as haemoglobin A1C test.
- The A1C aim for most persons with diabetes is to keep it around 7%.
Control Blood Pressure And Cholesterol
- Eating well-balanced meals, exercising frequently, and reducing weight can all help in keeping blood sugar levels and cholesterol under control.
- Medication is sometimes required as well.
Quit Smoking
- Smoking raises your chances of developing diabetes problems including diabetic retinopathy.
- Therefore, try to quit smoking or you may take some tips from your doctor for quitting smoking.
Consider Vision Changes
- If your eyesight suddenly changes or becomes blurry, spotty, or foggy, see your eye doctor immediately once.
- Keep your eye specialists informed about the frequent observations.
When To See An Eye Doctor
The best approach to avoid vision loss is to keep your diabetes under control. Even if your vision appears to be good, consult your eye doctor for an annual eye check with dilation if you have diabetes.
Diabetic retinopathy is more likely to happen if you get diabetes while pregnant (gestational diabetes). Else, if you already had diabetes before becoming pregnant. If your eyesight changes suddenly or becomes blurry, spotty, or foggy, see your eye doctor immediately.
A Word From MantraCare
Do you want to get rid of diabetes? Join our online diabetes consultation program and reverse your Diabetes naturally through lifestyle changes such as a Personalized Diet plan, Exercise, dieticians, and health coaches.