Continuous glucose monitors (CGM) are a modern technological breakthrough in the world of diabetes management. These sensors measure your blood sugar and show it on a screen. They tell you when the levels go up or down. No more finger-prick blood tests. No more worry about your correctly calibrating meters. CGM’s are the best way to tell how your body is responding. You can see if insulin or medication is working. The article below is about some of the advantages of using a continuous glucose monitor.
Contents
- 1 What are Continuous Glucose Monitors?
- 1.1 How Do Continuous Glucose Monitors Work?
- 1.2 Types Of Continuous Glucose Monitors
- 1.3 Benefits Of Continuous Glucose Monitors
- 1.4 How CGMs Change Life with Diabetes
- 1.5 CGM Systems Currently Available
- 1.6 How Do I Get a CGM?
- 1.7 Who Should Use CGMs?
- 1.8 Is there any risk?
- 1.9 Can CGMs replace fingerstick tests?
- 2 Conclusion
What are Continuous Glucose Monitors?

Continuous glucose monitors (CGM) are devices that measure the sugar level of your blood every moment. You have a machine that tells you how much glucose is in your body. It will tell you how different things affect your health. Your doctor can use this information to adjust insulin doses so they are more precise.
A continuous glucose monitor is better than a standard blood test. A continuous glucose monitor can give you results in 20 minutes and it gives them all day. CGM is like a watch. It tells you what’s happening inside your body. Diabetes can be hard to manage. You might not know how it is doing with just guessing or estimating things. But with this technology, you will know the truth about your diabetes that changes your life every day.
How Do Continuous Glucose Monitors Work?
A continuous glucose monitor has three parts. It has a sensor that you put under your skin. A pacemaker is a device that helps your heartbeat. It is put on the outside of the body and sends signals back to it to help it work. Finally, there is a wire that goes between them that sends signals back and forth. This sensor is small and thin and it can measure your blood sugar all day and night. It sends the information to a remote monitor. A transmitter is about half an inch long. It needs to be changed every five days. It is smarter than carrying around heavy machines with tubes of blood which used to take readings.
Types Of Continuous Glucose Monitors
There are two kinds of CGM devices: one goes below the skin and is put in by a doctor. The other kind sits on your arm and you can take it off or change it if you need to. For people who have Type I Diabetes, there are other systems that they can try. If the FDA approves these, then it could change their life. There are some things you should know about continuous glucose monitors:
Subcutaneous devices

They last for a long time and they are easy to use. You don’t need to keep taking blood tests or finger sticks so often anymore. But it is difficult to put the sensor under your skin. This means that you need a doctor to do surgery on you. The doctor will put in a device that can keep the sensor in for you.
Transdermal devices

These sensors work on top of your body’s surface with no needles involved at all; you just stick them right onto your arm (similarly to when you get tested using glucose test strips). This system is good, but you might get scared when it’s on your arm. It will bother you if many things happen at the same time like working out, showering, and swimming. But this will get better as technology advances.
Benefits Of Continuous Glucose Monitors
People who have diabetes do not get to enjoy the benefits of modern technology. Some of the advantages include:
- Accurate information: CGM gives you an accurate look at what’s happening in your body all day long without disrupting daily activities like eating and sleeping if it is worn correctly. People can take control of their disease by using this amazing tool provided free by Dexcom.
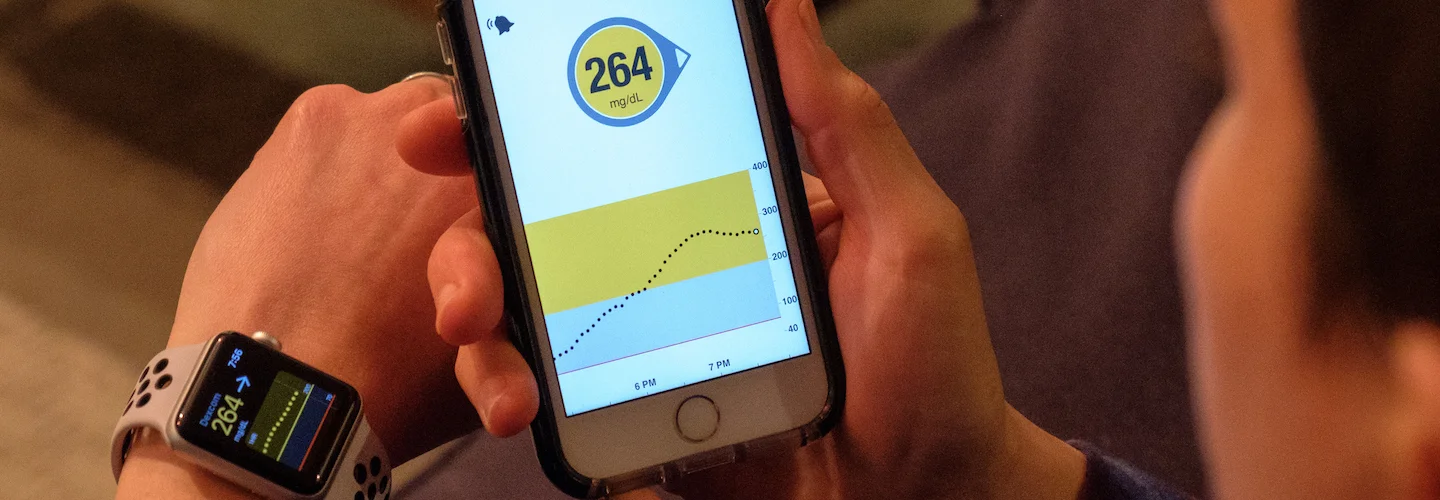
- Dexcom G-series Mobile app: This app makes it easy for people to see how they’re doing before meals or after exercise. The app is free for people in the United States to download. You can get it from Apple Store or Google Play.
- Bolus Advisor: This feature lets you have an idea of what your insulin doses are doing so that you can reduce high blood sugars during mealtime (which prevents future complications). Experts say that if people rely more on a CGM, their diabetes will be better controlled. They will need fewer visits to the doctor’s office. This could save up to $100 per month. Dexcom G-series already has FDA approval. Other continuous glucose monitors still need to go through the same process. Insurance companies may cover some of the costs now that Dexcom G-series has this approval.
This is just one of many advancements for people who have diabetes. The technology could help millions of people around the world. CGM devices are small gadgets that can be bought at the pharmacy. They help patients with diabetes. Patients might also get a discount if they contact their insurance company before buying these things. Dexcom has been making the monitors for a long time. They have made 500,000 of them since they first came out in 2008. I hope that there will be more coming soon because it would mean cheaper prices than the competition.
How CGMs Change Life with Diabetes
• CGM stands for continuous glucose monitor. This is a small device that you attach to your body. It is a machine that takes the sugar from your blood every few minutes. It does this all day, every day.
• CGMs are a new thing that can help people with diabetes. It is a way for people to find out how their blood sugar levels are without having to poke their skin.
• Most systems currently on the market are only accurate up to +/- 20% of a lab test.
• The FDA wants all devices that say they measure blood sugar to be accurate. They consider CGM devices to fall under this category.
CGM Systems Currently Available
There are many different CGM systems available in the market. Some of them are:
Dexcom G-Series CGM
This device is a small plastic strip with a sensor. It measures the glucose concentration in the interstitial fluid between cells.
Medtronic Minimed Enlite Sensor
A flexible, short wire is attached to the adhesive disposable patch. Electrodes are inside the wire. They detect glucose levels as they move across fluids or blood.
Senseonics Eversense XL System
An implantable system under the skin using 150-200 microneedles containing both a sensing mechanism and a micropump for delivering insulin. It can measure sugar concentrations noninvasively via subcutaneous fluorescence every few minutes continuously over a period of at least 90 days.
Abbott’s Freestyle Libre Flash Glucose Monitoring System
A small round patch is worn on the back of your upper arm that measures glucose levels using a tiny sensor inserted just below the skin and attached to a disposable reader device about as big as a mobile phone. The monitor also uses Bluetooth for data transfer so you can read results from up to 20 feet away through an app on your smartphone or tablet. Some products are not FDA-approved but have been available in other countries for some time, including:
GlucoWatch Biographer by Cygnus Inc.
An implantable system that used reverse iontophoresis to draw interstitial fluid into an implanted chamber containing biosensor enzymes. The fluid was then mixed with an enzyme substrate solution, which is continuously pumped through the chamber by a small pump in order to react within it and produce a proportional electrical current that can be measured without piercing the skin.
GlucoSentry
An implantable device currently available outside of the United States for measuring glucose levels in interstitial fluids between cells using reverse iontophoresis technology developed by Cygnus Inc., but has seen limited use due to problems with sensor accuracy at high glucose concentrations (the target range being 100-400 mg/dL) and a lack of U.S. Food and Drug Administration approval for use as a medical device.
How Do I Get a CGM?
If you are already using insulin to manage your diabetes, make sure that you talk with your health care providers about whether or not a CGM might be right for the type of patient you are.
Depending on insurance coverage and financial resources, some patients may find they can get one through their clinician’s office at little to no cost; others may have to pay out-of-pocket (or come up with another way to cover it), which typically costs between $1500-$3000/year.
Who Should Use CGMs?
• Because these devices provide real-time information on blood sugar levels throughout the day and night without needing an invasive procedure like traditional glucose monitoring methods, those who wear them usually experience fewer high or low blood sugar levels.
• Thus, those who use insulin and/or glucose-lowering medications to manage their diabetes may benefit from using a CGM as well.
Is there any risk?
In general, CGMs are safe for most people with or without diabetes. However, you should take the same precautions that you take when engaging in physical activity: Have an extra source of blood glucose available if needed (e.g., hard candy, juice) just in case your CGM does not detect a low immediately; wear medical identification jewelry or carry some sort of card explaining what type of device is on your body if it gives off an electrical signal since others might mistake this for a pacemaker or other electronic implant device). Also, make sure you tell your doctor if you have a history of skin irritation or other problems at the site where your device is.
In regard to software, manufacturers recommend that a clinician should train the users on proper use and troubleshooting before using it alone without direct supervision from someone who understands how CGMs work. In addition, they should be aware that CGM accuracy can vary depending upon user technique (e.g., insertion procedure), calibration timing/frequency, environmental factors such as body temperature, exercise intensity level, and even food intake within a few hours before testing blood glucose levels. Finally, know what type of signals mean for each system so you don’t mistake normal sensor function for something else; in some cases, this may mean delaying treatment until more information is available.
Can CGMs replace fingerstick tests?

No, they can’t; each is useful for different things and it’s important to know the limitations of both devices in order to maximize your diabetes management experience. Since traditional glucose monitoring requires that blood should draw from a fingertip or earlobe (or on rare occasions, another site), this allows you to track how certain foods/beverages affect your blood sugar levels over time so you know which ones are most appropriate for controlling symptoms at particular times throughout the day. For instance, if testing reveals that eating pasta causes your numbers to go too high soon after finishing an entire plateful of spaghetti al dente with meat sauce instead of just half like before, then these findings will help you adjust your meal plan accordingly.
Conclusion
The CGM is a sensor that one can use to measure glucose levels in the blood. It’s also an “artificial pancreas”. The University of California, San Francisco, designed this device and tested it on animals for years. Researchers are hoping it will help diabetics better monitor their health and avoid some dangerous side effects like hypoglycemia or hyperglycemia. If you’re living with diabetes and want more information about this technology, we encourage you to talk to your healthcare provider today! We’ll tell you what they say when we hear back from them!
Do you want to get rid of diabetes? Join our online diabetes consultation program and reverse your Diabetes naturally through lifestyle changes such as a Personalized Diet plan, Exercise, dieticians, and health coaches.


