Contents
- 1 What Is Short-acting Insulin?
- 2 How Does Short-Acting Insulin Work?
- 3 Difference b/w Long-acting & Short-acting Insulin
- 4 When To Use Short-acting Insulin?
- 5 Who Should Not Take Short-acting Insulin?
- 6 How Do I Use Short-acting Insulin?
- 7 When Should I See My Doctor?
- 8 How Do I Take Insulin?
- 9 What Time Of Day Should I Take My Dose?
- 10 Things To Consider Before Taking Insulin
- 11 Advantages Of Taking Insulin
- 12 Disadvantages Of Taking Insulin
- 13 A Word From Mantra Care
What Is Short-acting Insulin?

Short-acting insulin is a type of insulin used to treat diabetes. This class of insulin lowers blood sugar for three to six hours after injection, depending on the dosage. Unlike long-acting insulin, which is injected once or twice daily, short-acting insulin can be taken as needed to cover meals or snacks that are higher in carbohydrate content.
Insulin is a hormone produced by the pancreas that helps turn sugar from food into energy the body can use. In people with diabetes, either their own pancreas doesn’t make enough insulin or their cells don’t respond appropriately to insulin and cannot get sugar out of the bloodstream. As a result, sugar builds up in the blood causing high blood glucose levels which is extremely dangerous. If left untreated, this will cause serious damage to many parts of the body including the heart, eyes, kidneys, and nerves over time.
People with diabetes need to take insulin, but not all types of insulin are the same. There are two main types of insulin: long-acting and short-acting. The long-acting injection works once or twice a day and lasts up to 24 hours. The patient should prefer a Short-acting injection before meals and snacks that contain carbohydrates, and it lasts for three to six hours after injection. There are short-acting insulins available including; Neutral (NPH), Lente, Ultralente, and Detemir.
How Does Short-Acting Insulin Work?
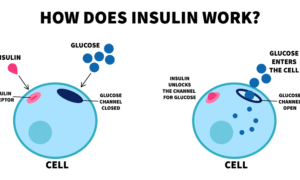 Insulin is needed to allow glucose to enter cells so they can use it for energy. But when you have type 1 diabetes, your body stops making the insulin it needs. Short-acting insulin works by replacing what’s missing so that glucose can get into your cells and lower your blood sugar.
Insulin is needed to allow glucose to enter cells so they can use it for energy. But when you have type 1 diabetes, your body stops making the insulin it needs. Short-acting insulin works by replacing what’s missing so that glucose can get into your cells and lower your blood sugar.
Short-Acting Insulin: Short-acting insulin is a type of insulin that lowers blood sugar for three to six hours. It is used to treat diabetes in patients who need to take insulin but can’t or don’t want to take it 24 hours a day. Short-acting insulin can be taken as needed, instead of taking it once or twice daily like long-acting insulin. This type of insulin is also injected before meals and snacks containing carbohydrates and lasts for three to six hours.
Short-acting insulin is a type of fast-acting insulin that only lasts a short time in the body. It’s taken to control blood sugar levels after eating or before going to bed at night. Short-term/Rapid-acting insulin has an onset of about 1/2 hour and lasts from 2 1/2 hours to 3 hrs. This makes it the ideal type of insulin for meals or snacks which you know will happen very close to mealtimes. Insulin acts differently on different people so you should consult with your doctor before taking any medication especially if it’s new for you since they’ll have a better idea as to what dosage may work best for you – this will also help them avoid giving you any medication which will be too much for you.
Difference b/w Long-acting & Short-acting Insulin
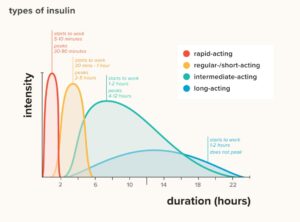
The difference between long-acting and short-acting insulins is the time span they work. Long-acting provides coverage for up to 24 hours whereas short-acting only lasts 3-6 hours.
People with diabetes need to take insulin, but not all types of insulin are the same. There are two main types of insulin: long- and short-acting. Long-acting is injected once or twice a day and lasts up to 24 hours, whereas short-acting is taken before meals and snacks that contain carbohydrates and it lasts for three to six hours after injection.
Short-acting insulin is always taken shortly before eating or after eating to manage blood-sugar levels. It’s also used with long-acting insulin (Levemir) in many cases. Short-acting insulins are usually for people who take three or more injections of insulin per day because they have a fast onset and shorter duration of action than other types of insulin. The most common side effects that affect less than 1% of users are hypoglycemia, allergic reactions, weight gain, swelling at injection sites, skin problems including redness, irritation, and itching as well as testicular pain.
The absorption rates change depending on where you inject it. If you take it under your skin, there is a slower absorption rate compared to when you take it under your tongue (sublingual). If you want fast-acting insulin, you’ll need to take it sublingually.
You should not mix this two insulin together. Doctors recommend that you should not mix the two types of insulin together as there are different absorption rates at play. If you do so, you run the risk of experiencing hypoglycemia (low blood sugar).
When To Use Short-acting Insulin?
Short-acting insulins are generally recommended for people who take 3 or more injections per day. Since they have a fast onset and shorter duration of action than other types of insulins. The most common side effects that affect less than 1% of users include hypoglycemia or low blood sugar. And allergic reactions such as swelling and itching at the injection site, weight gain, skin problems such as redness and irritation at the injected site, and testicular pain. Non-diabetics should take note though that while insulin injections will raise your blood glucose levels they also lower your ketones (which is why diabetics using insulin need to be aware of their ketone levels).
You should only use this type of insulin as needed, such as if you’re having a meal that’s higher in carbohydrate content than usual. Your doctor will let you know how much to take based on your current dose of long-acting insulin. If you miss a dose or use too much, you could go into diabetic ketoacidosis (DKA), which is dangerous for your health.
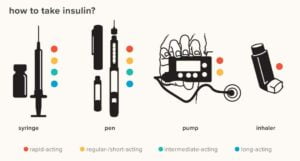
If you need to inject quickly before eating, try using an insulin pen instead of injections with syringes.
Who Should Not Take Short-acting Insulin?
For people who are allergic to insulin, taking medications like acetaminophen (Tylenol) can cause liver damage, and those who have diabetic ketoacidosis (DKA) shouldn’t take this type of insulin. Short-acting insulin is also contraindicated in patients with some specific diseases. Like hypoglycemia unawareness, thrombocytopenia (low platelet count), acute stress reaction, heart failure, active cancer, acute respiratory failure, coma, alcohol intoxication, untreated acidosis, diabetic coma, insulin-dependent diabetes mellitus (IDDM), low potassium in the blood, ketoacidosis, kidney or liver disease and pediatric patients who are critically ill.
How Do I Use Short-acting Insulin?
Before injecting yourself with short-acting insulin, check that it is not discolored or cloudy. Make sure you’re using an approved brand of insulin. Speak to your doctor before switching to a different kind of insulin. Choose an area on your stomach, upper thighs, or the back of your arms and rotate injection sites to prevent infection. Hold the needle at a 90° angle and insert it into your skin by pushing it in swiftly. Once the needle is inserted, push down on the plunger so insulin can enter your body. Pull out the needle once you have injected all of the insulin.
When using injections with syringes, store them in a cool place but not in direct sunlight or inside a refrigerator. You should also keep this type of insulin away from moisture and do not use any after its expiration date. Keep short-acting insulin outreach from children as it can be harmful if taken inappropriately.
Do not share your needles or syringe with anyone. It can lead to infection and other health problems for both you and the person injecting themselves. Dispose of used needles in a puncture-proof “sharps container”. If you need help buying insulin, call your local pharmacist, diabetic educator, or primary care doctor. Try talking to your insurance company about coverage for insulin supplies.
When Should I See My Doctor?
If you are using this type of insulin as needed, call your doctor if the blood sugar level becomes too low (hypoglycemia). Your dose may need to be adjusted. Also seek medical attention if it is so high that complications arise like diabetic ketosis (DKA) where the body produces too much acid and the blood becomes highly acidic, putting you at risk for coma.
Symptoms of DKA include:

- Nausea and vomiting
- Rapid breathing
- Dry skin
- Increased thirst and urination
- Sudden weight loss
If you notice signs or symptoms of ketoacidosis such as confusion, drowsiness, increased thirst, increased urination; nausea; stomach pain; vomiting; shortness of breath; tiredness, and trouble breathing while sleeping (with a possible change in the color of your breath), seek medical attention immediately. Insulin is a hormone produced by the pancreas that helps turn sugar from food into energy the body can use. In people with diabetes, either their own pancreas doesn’t make enough insulin or their cells don’t respond appropriately to insulin and cannot get sugar out of the bloodstream. As a result, sugar builds up in the blood causing high blood glucose levels which is extremely dangerous. If left untreated, this will cause serious damage to many parts of the body including the heart, eyes, kidneys, and nerves over time.
How Do I Take Insulin?
Usually, taking short-acting insulin is not a tough task. A person can inject it into their skin or stomach. You can inject short-acting insulin into your skin or stomach. Some people mix it with longer-acting insulin and take it as one injection, but this is not recommended for everyone. We recommend you talk to your doctor first before doing so.
And for measuring the dose of insulin, a very thin needle attaches to a syringe and we use that to measure out the appropriate dose of insulin (ranging from 0.1 ml up to 1 ml).
Completing your injections is important because it helps to regulate the levels of insulin in your blood. If you don’t complete all of your injections, then there’s a risk that you’ll develop high blood sugar which will put you at greater risk for developing other problems such as eye or kidney issues.
What Time Of Day Should I Take My Dose?
 You can take your dose anytime during the day, but some people like to split their doses up to help cover food intake over the course of the day. It usually takes about 3 hours for insulin to start working after injecting it. Depending on what type of insulin is prescribed for use. Doctors will usually recommend that you take your second dose at either lunch or dinner.
You can take your dose anytime during the day, but some people like to split their doses up to help cover food intake over the course of the day. It usually takes about 3 hours for insulin to start working after injecting it. Depending on what type of insulin is prescribed for use. Doctors will usually recommend that you take your second dose at either lunch or dinner.
Short-acting insulin is a type of insulin that can be taken at mealtimes. It has a duration of action from 3 to 5 hours, which means it will last for about 4 or more hours after you eat. Short-acting insulin differs from basal and intermediate insulins in the way they are entering your body. With short-acting insulin being injected before eating while other types are taken as an injection 2 times per day. If you have been prescribed this kind of medication by your doctor. Make sure to follow their instructions carefully when administering them.
Things To Consider Before Taking Insulin
 You always need to be aware of what you’re eating when you take insulin. Some people might be able to tolerate it well but others, not so much. Make sure you read up on any foods you want to consume and find out if they are good for insulin users.
You always need to be aware of what you’re eating when you take insulin. Some people might be able to tolerate it well but others, not so much. Make sure you read up on any foods you want to consume and find out if they are good for insulin users.
And most people can still play sports with their injections. Just make sure your doctor is aware of it beforehand. It’s important to note that exercise may affect the absorption rates of the insulin high in carbs or sugars could throw off blood glucose levels, especially if you’re just starting out with your injections.
Also, you should take a physical examination before using insulin. Yes, it is important that a doctor or a specialist approves of the use of insulins for each person. It’s also vital to have regular check-ups so as to monitor blood sugar levels and any possible side effects from taking insulin.
When it comes to pregnant women who have diabetes, They have to be extra careful. Pregnant women usually require very low doses (less than 1 unit) of short-acting insulin per day due to changes in their body composition – many don’t even need it at all.
The use of short-acting insulin is pretty simple. However, there are many medical things that can get in the way of a person being able to take their injections regularly and effectively. If someone cannot take their injections regularly then they’re going to have problems managing their disease and making sure that their condition doesn’t get worse.
Advantages Of Taking Insulin
Many people who suffer from diabetes take insulin in order to regulate their blood sugar levels. This can be a challenge because of the unpredictability of diabetes and the number of side effects they may experience including hypoglycemia or hyperglycemia. In spite of this, taking insulin is still a favorable option for many because it offers them a convenient way to manage their condition without any complications. Some common advantages that they enjoy when taking insulin include:
- Regularisation of blood-glucose levels
- Reduced risk of health complications
- Simplicity– there’s no need for daily injections or dosage calculations
- Affordability – most people have insurance coverage.
The only disadvantage of taking insulin is that it can cause low blood sugar levels. That can lead to problems with shakiness, hunger, sleepiness, or confusion. However, this side effect is easily managed by increasing your dosage of insulin or giving yourself a snack before each injection.
Disadvantages Of Taking Insulin
The most common side effects that affect less than 1% of users include hypoglycemia or low blood sugar, allergic reactions. Such as swelling and itching at the injection site, weight gain, skin problems such as redness and irritation at the injected site, and testicular pain. Non-diabetics should take note though that while insulin injections will raise your blood glucose levels. They also lower your ketones (which is why diabetics using insulin need to be aware of their ketone levels). While some people might find it difficult to give themselves injections, for others, it’s not as bad.
Side Effects
People with diabetes need to take insulin. Side effects of this type of insulin include hypoglycemia (low blood sugar), weight gain, and low potassium levels in the blood. If you experience these, contact your doctor right away:
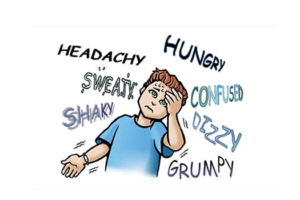
Hypoglycemia/Low blood sugar level: This occurs when blood sugar drops below normal and can cause dizziness, confusion, drowsiness, or seizures. If you constantly have lows then there might be an issue with the way that you’re executing your injections. Consult with your doctor and ask how often to take the doses. And what you can do to make them more effective in regulating your blood levels.
Weight gain: An increase in appetite is common with this type of insulin, which may lead to weight gain.
Low potassium levels in the blood: Symptoms include nausea, vomiting, weakness, and/or tingly feeling around the mouth.
Itching, swelling of the site: Redness and soreness along with discoloration on the site where insulin was injected. This is usually because of having a poor diet or not taking proper care of yourself after taking an injection. However, these symptoms will usually go away on their own. Otherwise, contact a medical professional for assistance.
Short-acting insulin is a type of fast-acting insulin that only lasts a short time in the body. Insulin injection helps control blood sugar levels after eating or before going to bed at night. Short-term/Rapid-acting insulin has an onset of about 1/2 hour and lasts from 2 1/2 hours.
A Word From Mantra Care
If you are looking for more information on this topic or on Diabetes treatment, Online Therapy, Hypertension, PCOS treatment, Weight Loss, and Physiotherapy, please visit mantracare.org or feel free to reach out to us at +91-9711118331 or email at contact@mantracare.org. You can also download our free Android App or IOS app.
Here at Mantra Care, we have an incredibly skilled team of health care professionals and coaches who will be happy to answer any questions and provide further information so you know what’s best for your unique needs.