Type 1 diabetes is one of the most debilitating diseases in the world. It is a type of autoimmune disease that affects insulin production in your body, making it difficult to regulate blood sugar levels. The type 1 diabetes cure has been at the forefront for decades but still, no success story has emerged yet. Many organizations and researchers are working on finding a type 1 diabetes cure every day with little to no progress made so far. If you want to know more about type-1 Diabetes, Read more in this article.
Contents
What is Type 1 Diabetes?
type one diabetes is an autoimmune disease that causes your body to lose the ability to regulate blood sugar. Type two diabetes, on the other hand, results when you can’t produce enough insulin or cells stop responding to it.
When beta cells in the pancreas are destroyed. The body is unable to produce enough insulin. Insulin is a hormone that the body needs to regulate blood glucose levels (also known as blood sugar) and is produced by beta cells in the pancreas.
Type 1 diabetes is most often is present by an immune system reaction. The body assaults its insulin-producing beta cells in the pancreas as a result of this reaction. It typically affects youngsters and young adults, although it can happen at any age.
Insulin and Diabetes
Insulin allows food carbohydrates to enter the body’s cells for them to create energy. If glucose cannot get into these cells, too much sugar will accumulate in the circulation, resulting in hyperglycemia. It will eventually cause harm to the entire body.
These cells will also have insufficient glucose in their system, which can lead to tiredness and other problems.
Type 2 diabetes can be prevented through lifestyle modifications, but type 1 diabetes cannot. There is currently no cure, however, there are treatments that may help manage it.
According to statistics from 2016, there are around 1.3 million adults in the United States who have type 1 diabetes, accounting for about 5.8% of all people with diabetes in the country.
Symptoms of Type 1 Diabetes

The symptoms of Type 1 diabetes generally appear after a few days to weeks.
. They include:
- increased hunger and thirst
- frequent urination
- blurred vision
- tiredness and fatigue
- weight loss without an apparent trigger or cause
Anyone who experiences these symptoms should immediately see a doctor or their healthcare team. A variety of issues can develop with time, producing a range of other symptoms.
The Honeymoon Phase of Type 1 Diabetes
When a person has diabetes, his or her body may continue to make insulin for some time.
It’s common for individuals with diabetes to have high blood sugar levels when they first start using insulin, especially if they are taking an emergency shot. Diabetics’ bodies respond differently to the hormone – in some people, the surge can last days or weeks. Meanwhile, their insulin levels may fluctuate during this time. They might require fewer insulin injections. the doctors call this phase the honeymoon phase.
It’s common for patients to boost their insulin doses gradually over time, thinking that if they do so, the disease will improve. This is rarely the case, though.
During this time, people should continue to communicate with their healthcare team and follow the established treatment strategy.
Causes for Diabetes
Causes for type one diabetes include genetics and environmental factors. It is unclear why these contribute to the development of type one but we must do what we can to reduce our risk. Type two diabetes on the other hand has a very simple cause: obesity.
Further Causes
In type 1 diabetes, beta cells are damaged, causing the mechanism to fail. Because insulin isn’t there to facilitate glucose transfer into your cells, it doesn’t enter. Instead, it accumulates in your blood and your cells starve. This results in high blood sugar, which can lead to:
- Dehydration is the condition in which your body loses more water than it takes in. You pee more when there’s extra sugar in your blood since this is your body’s method of eliminating it. Because a lot of water exits with that urine, your body will become dehydrated.
- Losing weight is easier with a smaller size. When you pee, glucose is excreted and calories are lost as a result. Many people with high blood sugar suffer from dehydration as well. Dehydration has an impact as well.
- DKA, or diabetic ketoacidosis, is a serious condition that can be deadly if not treated promptly. Your body breaks down fat cells rather than obtaining enough glucose for energy if it cannot obtain enough glucose. Ketones are in production as a result of this. To assist out, your liver releases the sugar it has stored. However, without insulin, this type of sugar cannot go into the cells. It accumulates in your blood, causing ketones to rise too high and become toxic.
- Damage to your body’s cells. High glucose levels in your blood can harm the nerves and small blood vessels in your eyes, kidneys, and heart over time. They can also contribute to increased odds of developing hardened arteries, or atherosclerosis, which can result in heart attacks and strokes.
However, even if you are at risk type one diabetes can be completely preventable. It doesn’t matter if you are genetically in predisposition to type one, there is still a lot that we all do every day that increases our chances of developing type one diabetes.
Diagnosis of Type 1 Diabetes

Diagnostic tests include:
- The A1C test measures the percentage of blood sugar linked to the oxygen-carrying protein in red blood cells (haemoglobin). The proportion of blood sugar bound to the oxygen-carrying protein in your red blood cells (haemoglobin) is measure by the A1C test. An A1C level of 6.5 per cent or higher on two separate tests indicates that you have diabetes.
- The presence of type-one diabetes is often in identification through routine screening in those who are particularly at risk. Such as children and young adults with a first-degree relative (parent or sibling) with type-two diabetes. However, type one can develop even if there is no family history.
Tests for Type 1 Diabetes
If the A1C test isn’t available, or if you have any of these circumstances that might render the A1C test unreliable — such as pregnancy or a rare form of haemoglobin (haemoglobin variant) — your doctor may use one of these strategies:
Random Blood Sugar Test
A random blood sugar test will be performed. A blood sample may be taken at any time for confirmation. Blood sugar levels are measured in milligrams per deciliter (mg/dL) or millimoles per litre (mmol/L). When coupled with any of the signs and symptoms of diabetes, such as frequent urination and excessive thirst, a random blood sugar level greater than 200 mg/dL (11.0 mmol/L) or symptoms or signs of hyperglycemia indicate type-one diabetes, and no further testing is needed.
A-C Peptide Test
A C-peptide test may be in use to aid in the diagnosis of type one diabetes when both A and B cannot be completed. This test measures the amount of insulin that is produced after a type-one diabetic has fasted for 12 to 14 hours. However, this type of testing can be used only in those who are at least 15 years old and it cannot rule out type-two diabetes-like A and B tests can.
Overnight Blood Sugar Test
A blood sugar test will be conducted after an overnight fast. Normal fasting blood sugar levels are under 100 mg/dL (5.6 mmol/L). Prediabetes is referred to when the fasting blood sugar level is between 100 and 125 mg/dL (5.6 and 6.9 mmol/L). If your two tests result in a diagnosis of type two diabetes, your doctor will need to know which type you have as a treatment for type two is different from type one.
Additional Testing
If you’re in diagnosis with type 1 diabetes. Your doctor may do blood tests to look for autoantibodies that are typical in type 1 diabetes. When the distinction between type 1 and 2 diabetes is unclear, these tests assist your doctor to recognize if someone has either form of the disease. The presence of ketones — by-products produced during fat metabolism — in your blood or urine, which often happens with type one diabetes, is another clue that type-one diabetes may be developing.
You will need to monitor your glucose levels regularly using either a fingerstick test meter kit or an auto-monitoring kit. You should also check for ketones when you experience symptoms of high blood sugar or hyperglycemia.
After the Diagnosis
You’ll typically visit your doctor about diabetes management. The doctor will check your A1C levels during these appointments. Your desirable A1C goal might be different depending on your age and other circumstances. The American Diabetes Association suggests that A1C levels should be below 7 per cent (estimated average glucose of 154 mg/dL; 8.5 mmol/L).
Testing for Type 1 Diabetes in Children
When type-one diabetes is diagnosed in someone under the age of 18, additional testing may be needed. For example, your doctor might order a magnetic resonance imaging (MRI) scan to look for evidence of type-two diabetes if you’re obese or have symptoms that don’t easily fit type one.
A1C testing, as compared to multiple daily blood sugar tests, is more accurate at determining how effectively your diabetes treatment plan is working. An A1C level of over 9 per cent may suggest the need for a change in your insulin regimen, meal plan, or both.
The doctor will also take blood and urine samples regularly to assess your cholesterol levels, thyroid function, liver function, and kidney function. The doctor will also check your blood pressure and the locations where you test your blood sugar and give insulin.
Treatment for Type 1 Diabetes
Treatment for type 1 diabetes includes:
- Taking insulin
- Carbohydrate, fat, and protein counting
- Frequent blood sugar monitoring
- Eating healthy foods
- Exercising regularly and maintaining a healthy weight
The aim is to maintain your blood sugar levels as near to normal as feasible to avoid or postpone issues. The objective is usually to keep daytime blood sugar levels before meals between 80 and 130 mg/dL (4.44 and 7.2 mmol/L) two hours after eating, and post-meal readings no higher than 180 mg/dL (approximately 11 mmol/L).
Insulin and Other Medications
Anyone who has type 1 diabetes needs lifelong insulin therapy.
Types of insulin are many and include:
- Short-acting (regular) insulin
- Rapid-acting insulin
- Intermediate-acting (NPH) insulin
- Long-acting insulin
Humulin R and Novolin R are two examples of short-acting (daily) insulin. Insulins glargine (Lantus, Toujeo Solostar), lispro (Humalog) and aspart (Novolog) are rapid-acting insulins. Long-acting insulins include glargine (Lantus) and detemir (Levemir).
Insulin Administration
Insulin cannot be taken orally to lower blood sugar because stomach enzymes will destroy it, preventing its effectiveness. You’ll need an insulin pump or injections to receive it.
Insulin Injections
- You can administer insulin with injections or an insulin pen, which also works as a dosing device. To inject insulin under the skin, use a fine needle and syringe or an insulin pen. Insulin pens come in disposable and reusable models and resemble ink pens.
- If you get insulin injections, you’ll probably need a variety of types throughout the day and night. Multiple daily injections that combine long-acting insulin with fast-acting insulin mimic the body’s natural use of insulin better than previous insulin regimens that required just one or two shots per day. A regimen of three or more insulin injections a day shows to improve blood sugar levels more than injections of insulin alone.
Insulin Pumps
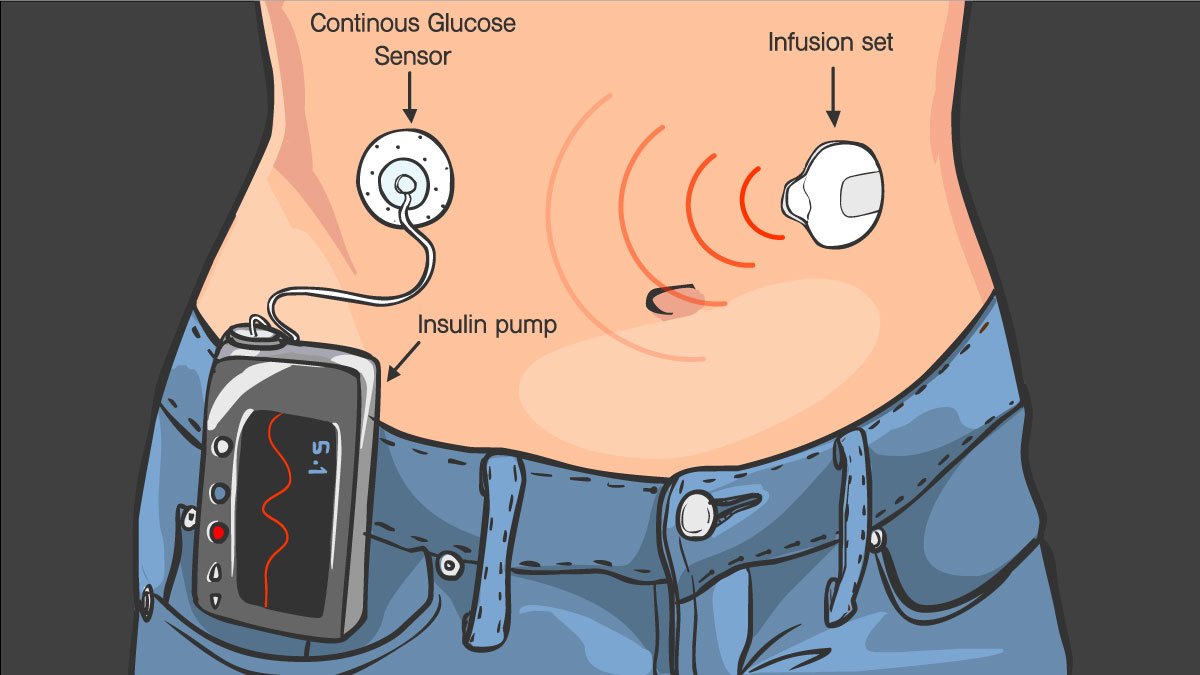
- A pump that is wearable outside of the body. This gadget, which resembles a smartphone, is attached to the outside of your body. A catheter with an insulin reservoir is inserted beneath the skin of your abdomen and connected to a pump via a tube. The pump is easy to carry in various locations, such as on your waistband, in your pocket, or attached to a belt.
- Some type of monitoring device is usually necessary when using insulin pumps, although the type will depend on where you decide to place your pump. The most common type of monitor has two parts: an infusion set with a short needle that inserts into the skin and connects to the catheter tubing under your skin; and a handheld reader that displays insulin infusion activity.
Wireless Pumps
- There’s a wireless pump alternative as well. You wear a pod with the insulin reservoir on your body that has a tiny catheter inserted beneath your skin. The insulin pod can be worn on your abdomen, lower back, or leg, or arm. A wireless gadget transmits signals to the pod, This is then in interpretation by a computer system.
- Pumps are in design to deliver a pre-programmed amount of fast-acting insulin automatically. Your basal rate is the steady dose of insulin that takes the place of whatever long-acting insulin you were using before.
- When you eat, the pump records the number of carbohydrates you consume and your present blood sugar level, and it provides you with a bolus dose of insulin to cover your meal and bring down your blood sugar if it goes too high.
According to certain research, insulin pumps may be more successful than injections in lowering blood sugar levels. Injections, on the other hand, can effectively maintain good blood sugar levels in many patients. A combination of an insulin pump and a continuous glucose monitoring (CGM) device might provide even better blood sugar control.
Artificial Pancreas
The Food and Drug Administration approved the first artificial pancreas for people with type 1 diabetes who are 14 years old or older in September 2016. In December 2019, a second artificial pancreas was given FDA approval.
The following is a description of close-loop insulin delivery. A continuous glucose monitor, which checks blood sugar levels every five minutes, is in link to the insulin pump. When the monitor shows that additional insulin is in need, the device delivers the appropriate dose.
There are currently more clinical trials involving artificial pancreas (closed-loop) systems.
Other Medications
Additional medications may also be in use to treat type 1 diabetes, such as:
- High blood pressure medicine. Angiotensin-converting enzyme (ACE) inhibitors or angiotensin II receptor blockers may be in use to preserve your kidneys’ health. Individuals with diabetes and blood pressures of 140/90 mm Hg or higher should take these medicines (mm Hg).
- If your doctor feels you have an increased risk for a cardiovascular event and that taking a baby aspirin or regular aspirin daily will help protect your heart, he or she should discuss the potential bleeding risk with you before administering.
Statin cholesterol-lowering medications. Due to the heightened risk of heart disease, cholesterol guidelines are typically more aggressive in people with diabetes. The American Diabetes Association recommends that low-density lipoprotein (LDL, or “bad”) cholesterol be below 100 mg/dL (2.6 mmol/L).
Women should have a high-density lipoprotein (HDL, or “good”) cholesterol goal of at least 60 mg/dL (to convert to mmol/L, multiply by 0.0259). Treatment goals for triglycerides should be below 500mg/dL as well.
Healthy Eating and Type 1 Diabetes

There is no such thing as a diabetes diet. It’s also critical to base your meals on high-quality, low-fat, high-fibre foods like-
- Fruits
- Vegetables
- Whole grains
Your dietitian will recommend that you cut back on animal products and refined carbohydrates, such as white bread and sweets. Even people who don’t have diabetes can benefit from this nutritious way of eating.
You’ll need to know how many carbohydrates there are in the meals you eat so that your insulin levels will be adequate for your metabolism. A certified dietitian can assist you in developing a meal plan that fulfils your needs.
Physical Activity
Everyone needs to exercise daily, and people who have type 1 diabetes are no exception. To begin, talk with your doctor first regarding whether or not you can work out. Then pick activities that you like, such as walking or swimming, and make them part of your routine. Every week, aim for 150 minutes of moderate-intensity activity.
Remember that physical activity lowers blood sugar levels. If you start a new exercise, check your blood sugar more frequently than usual until you understand how it affects your blood sugar levels. To compensate for the increased activity, you may have to alter your meal plan or insulin dosages.
Potential Future Treatments
Pancreas transplantation
- You would no longer require insulin after obtaining a successful pancreas transplant. Pancreatic transplants, on the other hand, aren’t always effective, and they come with significant risks. Because these dangers may be more severe than diabetes itself, pancreas transplants are mostly in use for individuals with extremely difficult-to-manage type I diabetes.
Islet Cell Transplantation
- The potential of islet cell transplantation is quickly approaching. Researchers are conducting trials to determine whether or not islet cell transplantation, which involves obtaining new insulin-producing cells from a donor pancreas, will be beneficial. Although this experimental treatment has had its difficulties in the past, improved techniques and stronger immunosuppressants to avoid islet rejection have allowed for a higher rate of success.
- Even if type I diabetes does not have a cure. It can be in treatment more effectively with an improvement in technology and research. This may make the disease easier to manage for type I diabetics. In one study done on mice, researchers were able to improve glucose metabolism in type I diabetic animals.
Coping with Type 1 Diabetes

Diabetes has the power to alter your emotions on both a direct and indirect level. Poorly controlled blood sugar can have an immediate influence on your mood by producing behavioural changes, such as irritability. There may be times when you are angry about your diabetes.
People with diabetes have an increased risk of depression and diabetic emotional distress, which might explain why many diabetes specialists include a social worker or psychologist on their team of care.
You might want to speak with other people who have diabetes. Online and in-person support groups are accessible. Members of the group frequently inform one another about the newest therapies, as well as offer their own experiences or useful information, such as where to find carbohydrate counts for your favourite takeout restaurant.
Conclusion
Type 1 diabetes can be cured through stem cell injections. These are the words of Dr Bruno Redondo, who is at the forefront of research in this field. His work has shown that injecting cells directly into a patient’s pancreas will stop it from attacking its beta cells and causing type 1 diabetes. This treatment also seems to have no negative side effects on people with type 2 diabetes or other autoimmune disorders. The main issue holding back these treatments is funding for more research trials, but researchers hope that they could potentially cure all forms of diabetes within 10 years if they receive enough support.
Do you want to get rid of diabetes? Join our online diabetes consultation program and reverse your Diabetes naturally through lifestyle changes such as a Personalized Diet plan, Exercise, dieticians, and health coaches.