Diabetic eye disease is a diabetic complication that can lead to blindness. This is a scary thought for anyone, but diabetic retinopathy and diabetic macular edema are the most common forms of diabetic eye disease.
In this blog post, we will go through what diabetic eye disease is, how it progresses from one form to another, and how one gets the treatment. With steroids or laser surgery?
Contents
- 1 What is Diabetic Eye Disease?
- 2 How Does Diabetes Affect My Eyes
- 3 Symptoms of Diabetic Eye Disease
- 4 When Should I See a Doctor
- 5 Causes of Diabetic Eye Disease
- 6 How Common is Diabetic Eye Disease
- 7 Who Can Develop this Disease
- 8 Diagnosis of Diabetic Eye Disease
- 9 Treatment of Diabetic Eye Disease
- 10 Prevention
- 11 Conclusion
What is Diabetic Eye Disease?

Diabetic eye disease (or diabetic retinopathy) is a complication of diabetes that affects the eyes. All people with type 1 or type 2 diabetes are at risk for diabetic retinopathy, but it can develop quickly in those who have poor control over their blood sugar levels and/or high blood pressure.
Diabetic retinopathy causes damage to small blood vessels in the retina of diabetic patients. These blood vessels can swell, leak fluid and bleed easily if their blood sugars are not well in control. Diabetic retinopathy is also in association with diabetic macular edema (damage to part of the retina called the macula), cataracts, glaucoma, high eye pressure, and blindness.
Diabetes is a chronic disease in which your body doesn’t produce or use insulin properly, resulting in high blood sugar levels. According to the Centers for Disease Control (CDC), about 30.3 million people in the United States have diabetes, and 90% of them have Type 2 diabetes — their bodies don’t react well to insulin and can’t keep blood sugar levels under control.
Type1 and Type 2 Diabetes
Type 1 diabetes, once known as juvenile diabetes or insulin-dependent diabetes mellitus (IDDM), results from the body’s failure to produce insulin in sufficient amounts. Type II diabetic is sometimes referred to as adult/noninsulin-dependent diabetes mellitus (NIDDM). It typically starts with an inability of the cells in the body to respond properly to insulin, a hormone that carries glucose from the blood into cells where it can be in use for energy. In Type II diabetes there is insufficient production of or response to insulin by the cells in the body and this leads over time to high levels of sugar in the bloodstream.
Furthermore, as many as one in four working-age individuals (those in their early 20s to early 60s) have Type 2 diabetes but are unaware of it. One doesn’t get diabetic eye disease overnight. It’s a slow process that can take years to develop.
How Does Diabetes Affect My Eyes
Diabetic Eye Disease is a condition that affects many people who have diabetes – it occurs when high blood sugar levels damage the tiny blood vessels in your eyes which leads to diabetic retinopathy, cataracts, and glaucoma.
People often think of diabetic eye disease as only affecting the eyes – however diabetic neuropathy, diabetic nephropathy, and diabetic dermopathy are also conditions that you may suffer from if your blood sugar levels aren’t well in control.
In the near term, high blood glucose is unlikely to cause vision loss. When individuals alter their diabetes treatment plan or medications, they sometimes have blurry vision for a few days or weeks. High glucose can cause changes in eye fluid levels or edema in the tissues surrounding your eyes, causing distorting vision. This kind of blurred vision is momentary and not associated with diabetic retinopathy.
However, eye disease is one of the long-term results of uncontrolled diabetes and happens when diabetic retinopathy develops in your small blood vessels – this damages them further which causes other diabetic symptoms to develop such as numbness or pain; loss of vision; high blood pressure; heart attack or stroke.
If your blood sugar levels remain high for a long period, it can harm the tiny blood vessels in the back of your eyes. This damage may begin during prediabetes when blood glucose levels are higher than normal but not high enough to diagnose as diabetes. Damaged blood vessels might leak fluid and cause swelling. New, weak blood vessels may form on the surface of your retina. This can lead to diabetic retinopathy, diabetic macular edema (DME), and diabetic vitreous hemorrhage.
Symptoms of Diabetic Eye Disease

Diabetic eye disease is a serious complication of diabetes but can be treated if diagnosed early enough.
Diagnosis for diabetic eye disease includes an examination of the retina by ophthalmologists or optometrists who specialize in diabetic eye care. If you have diabetic retinopathy or suspect that you may have diabetic retinopathy, consult with your eye doctor as soon as possible.
Diabetic retinopathy damages blood vessels in the retina, causing sight damage if left untreated. DME may develop as a result of it. More than 40% to 45% of people with diabetes have signs of diabetic retinopathy, although many do not realize it.
Symptoms include:
- Vitreous or internal floaters appear in your field of vision.
- If you’re experiencing blurred vision, check to see whether you have any internal floating objects.
- Colored spots that fade and become washed out are also possible. Dark areas within your field of view are common.
Diabetic macular edema is a condition in which fluid collects in the center of the retina, or macula. The macula, or center part of the eye, is responsible for sharp vision and most of our color perception. The following are some examples:
In the middle of your field of vision, you may notice blurring or waviness. Floaters are a common cause of seeing things in this way. Colors may appear faded or washed out.
Both types of diabetic eye disease can be treated. The treatment and efficacy of each therapy are determined by the severity of the problem.
When Should I See a Doctor
If you notice any unusual changes in your vision, such as flashes of light or many more spots (floaters) than usual, call a doctor right away. If it looks like a curtain is over your eyes, you should also see a doctor right now. These variations in your vision might be signs of a detached retina.
Causes of Diabetic Eye Disease
Diabetic Eye Disease (DED) is a condition that affects many people with diabetes, although it can also occur in those without the disease. DED includes all diseases of the cornea and retina caused by diabetic complications. The most common form of diabetic eye disease is diabetic retinopathy.
Diabetic Retinopathy

The retina NIH external link is the inner lining at the rear of each eye. The retina converts light into signals that your brain can interpret, allowing you to see the world around you. Diabetic retinopathy may be caused by damaged blood vessels, which can harm your retina and lead to diabetic retinopathy.
Blood vessels in diabetic retinopathy can weaken, swell, or leak into the retina at this stage. Nonproliferative diabetic retinopathy is a term to describe it.
If the condition gets worse, blood vessels may seal up, resulting in the formation of new blood vessels on the retina’s surface. This phase is proliferative diabetic retinopathy. These abnormal new blood vessels might result in significant vision problems if they grow larger.
Diabetic Macular Edemasa
This diabetic eye disease can cause loss of vision. It occurs when fluid builds up in the macula, which is located at the center of the retina and responsible for clear vision.
- When blood vessels get damaged because of diabetic retinopathy or uncontrolled diabetes then they swell. This results in the accumulation of excess fluid into macular edema lesions.
- It causes loss of central vision. Sometimes diabetic macular edema can lead to blindness if it is in combination with diabetic retinopathy or some other eye disease.
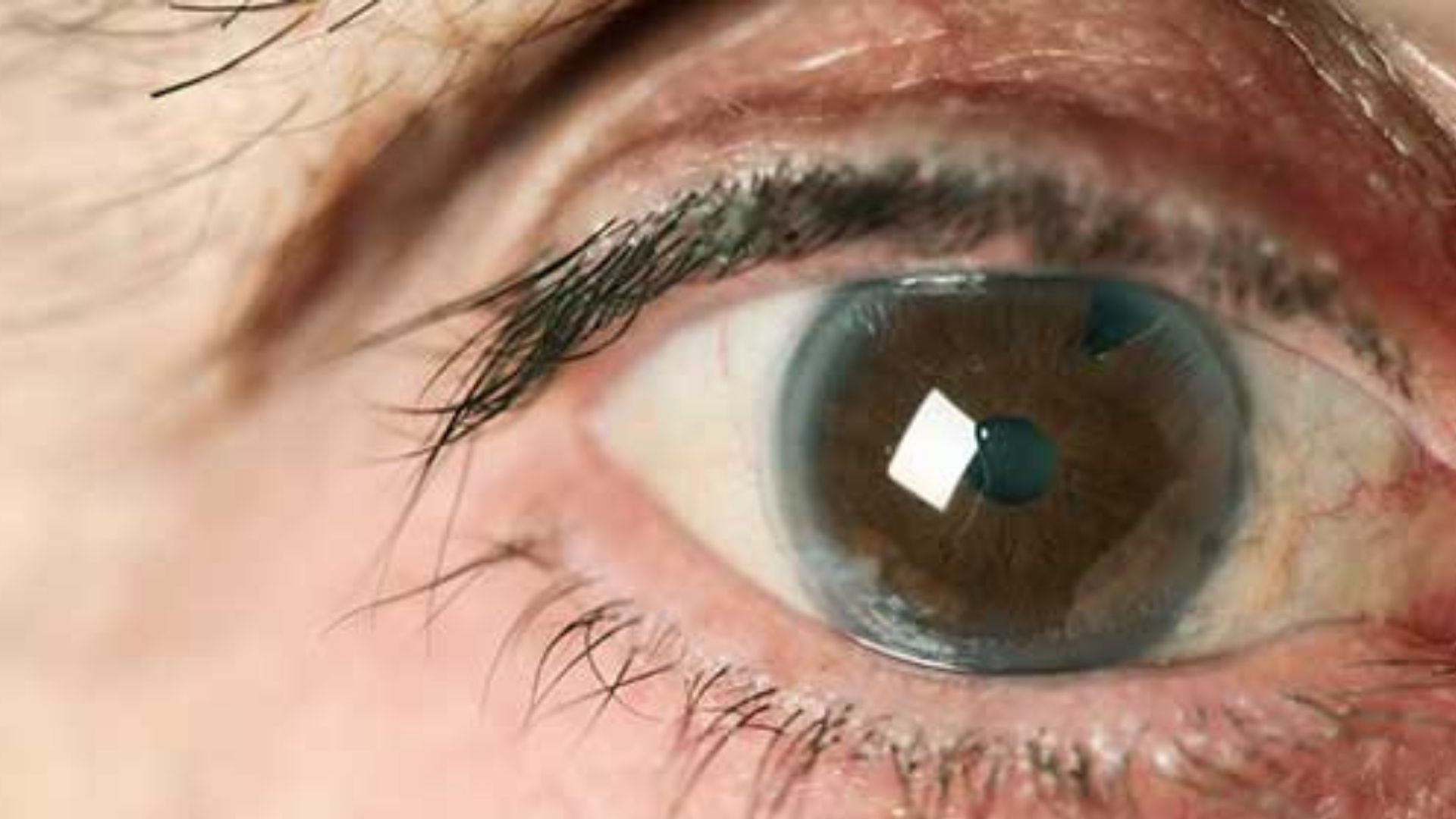
Glaucoma
Diabetic glaucoma occurs when high blood sugars damage the optic nerve, causing vision loss and eventually leading to blindness if not treated appropriately. While diabetic retinopathy is far more common than diabetic glaucoma, it does occur in diabetic patients as well. Diabetic vitreoretinopathy is a diabetic eye disease that can lead to blindness, too. Diabetic patients are at increasing risk for serious vision loss from diabetic vitreoretinopathy compared with other people without diabetes.
The consequences of glaucoma can be bad, depending on the type you have. Some types are-
Open-Angle Glaucoma
Open-angle glaucoma develops when the fluid in your eye – also called aqueous humor – doesn’t drain properly. If you have diabetic retinopathy, it could be due to this type of glaucoma. It can cause vision loss and blindness if not treated right away.
“Open-angle” implies that the iris meets the cornea at a wide and open-angle. Primary or chronic glaucoma is an umbrella term for open-angle glaucoma. It is the most prevalent form of glaucoma, affecting roughly three million people in the United States.
Angle-Closure Glaucoma
diabetic eye disease is not always straightforward, and sometimes other variables can cause the eyes to be in danger. One of these is angle-closure glaucoma, which happens when fluid cannot drain out of the eye properly because part of the drainage angle (where your iris meets your cornea) has closed up or become blocked. This can result in high pressure inside the eye, which damages your optic nerve and leads to vision loss if left untreated.
For diabetic individuals, this is particularly dangerous because diabetic retinopathy, diabetic macular edema (DME), diabetic vitreous hemorrhage, proliferative diabetic retinopathy are all contraindications for laser eye surgery that is normally used to unblock the drainage angle.
This means diabetic individuals who have developed this condition will need more invasive measures to treat their glaucoma, such as a surgical procedure called an iridotomy where small cuts are made around your pupil so pressure can be relieved.
The most common types of open-angle and angle-closure glaucoma are:
- Secondary Glaucoma
- Pigmentary Glaucoma
- Pseudoexfoliative Glaucoma
- Traumatic Glaucoma
- Neovascular Glaucoma
- Iaido Corneal Endothelial Syndrome (ICE)
- Uveitic Glaucoma
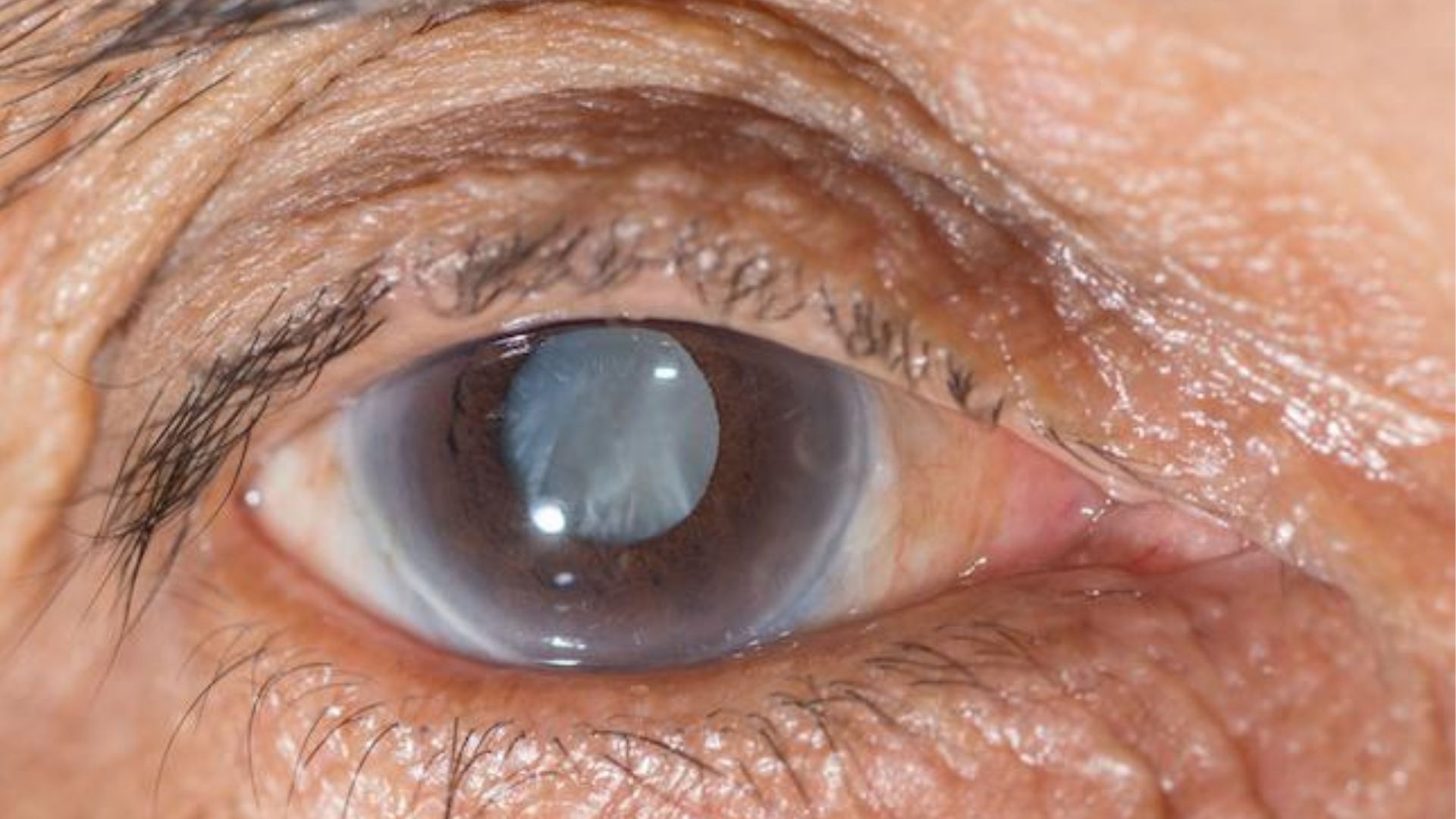
Cataract
The lenses of your eyes are transparent structures that help you see clearly — but they become hazy as we grow older. Cataracts, which are cloudy lenses, are more common in people with diabetes. People with diabetes have a greater chance than those without diabetes to acquire cataracts at an earlier age. High glucose levels may cause the lens of the eye to swell and press on other parts of your eyes.
Corneal Ulcers
Diabetic corneal ulcers are a common diabetic complication that can lead to blindness if not treated promptly. The term “cornea” refers to the clear outer covering at the front end of your eyeball, which is sensitive to light. Corneal ulcers are sores on the cornea that may be caused by diabetic neuropathy or poor blood flow in diabetic patients.
How Common is Diabetic Eye Disease
Diabetic retinopathy
About one in three adults who are 40 or older with diabetes already have some symptoms of diabetic retinopathy. 1 Diabetic retinopathy is the most prevalent cause of vision loss among individuals with diabetes. however, each person’s prospects are largely determined by careful attention. Early detection and treatment of diabetic retinopathy can reduce the chance of diabetic complications.
Glaucoma and Cataracts
Diabetes doubles your risk of developing glaucoma or cataracts, compared to someone who does not have diabetes.
Who Can Develop this Disease
Diabetic eye disease affects everyone with diabetes. The likelihood of developing high blood sugar and not treating it is greater than the risk of having high blood pressure and not treating it.
High blood cholesterol and smoking can also raise your risk of diabetic eye disease.
The disease can affect people of many different races, backgrounds, and social classes. African Americans, American Indians and Alaska Natives, Hispanics/Latinos, Pacific Islanders, and persons over the age of 60 are all at an increased risk of losing their sight or becoming blind due to diabetes.
If you have diabetes and become pregnant, your eyes can deteriorate rapidly during pregnancy. If you already have some diabetic retinopathy, it may get worse during pregnancy. Changes in your body that help your baby grow might put a strain on your eye’s blood vessels. Your doctor will recommend frequent eye check-ups throughout pregnancy to detect and treat any issues early.
Diabetic retinopathy can start as early as five years after your first diabetic symptoms. The earlier diabetic retinopathy is found, the more likely it can stop before you lose your sight and go blind. Diabetic eye disease does not have to lead to blindness if detected and treated quickly by a professional diabetic ophthalmologist
Diabetes that occurs only during pregnancy, called gestational diabetes, does not usually cause eye problems. Researchers aren’t sure why this is the case.
The longer you have diabetes, the more likely it is that you will develop diabetic eye disease.
Diagnosis of Diabetic Eye Disease
The greatest method to check for diabetes-related eye issues is to have a comprehensive dilated eye examination. To expand your pupils, your doctor will administer drops into your eyes. This allows the physician to examine a bigger area at the back of each eye with a specialized magnifying lens. For a few hours after a dilated exam, your vision will be blurry.
- Your doctor will also examine your eyesight and calculate the pressure in your eyes.
- Depending on your health history, your doctor may recommend additional tests.
- Most people with diabetes should see an eye care professional once a year for a comprehensive eye examination.
- Based on your type of diabetes and the length of time since you first learned you had it, your medical staff may propose something different.
Treatment of Diabetic Eye Disease
If you have diabetes, your doctor may suggest more frequent eye exams, as well as management of your diabetes. This entails monitoring your A1c, blood pressure, and cholesterol; as well as quitting smoking.
Advanced eye diseases may be in treatment by doctors with medicine, laser treatments, surgery, or a combination of both.
Medication
Your doctor may prescribe anti-VEGF medication, such as aflibercept, bevacizumab, or ranibizumab to treat your eyes. These medicines stop the formation of abnormal blood vessel growth in the eye. Anti-VEGF treatments can also help with fluid leaks, which aid in the treatment of diabetic macular edema.
During office visits, the doctor will administer anti-VEGF medication into your eyes. You’ll have numerous treatments during the first few months, followed by fewer treatments as you continue with therapy.
Laser Therapy
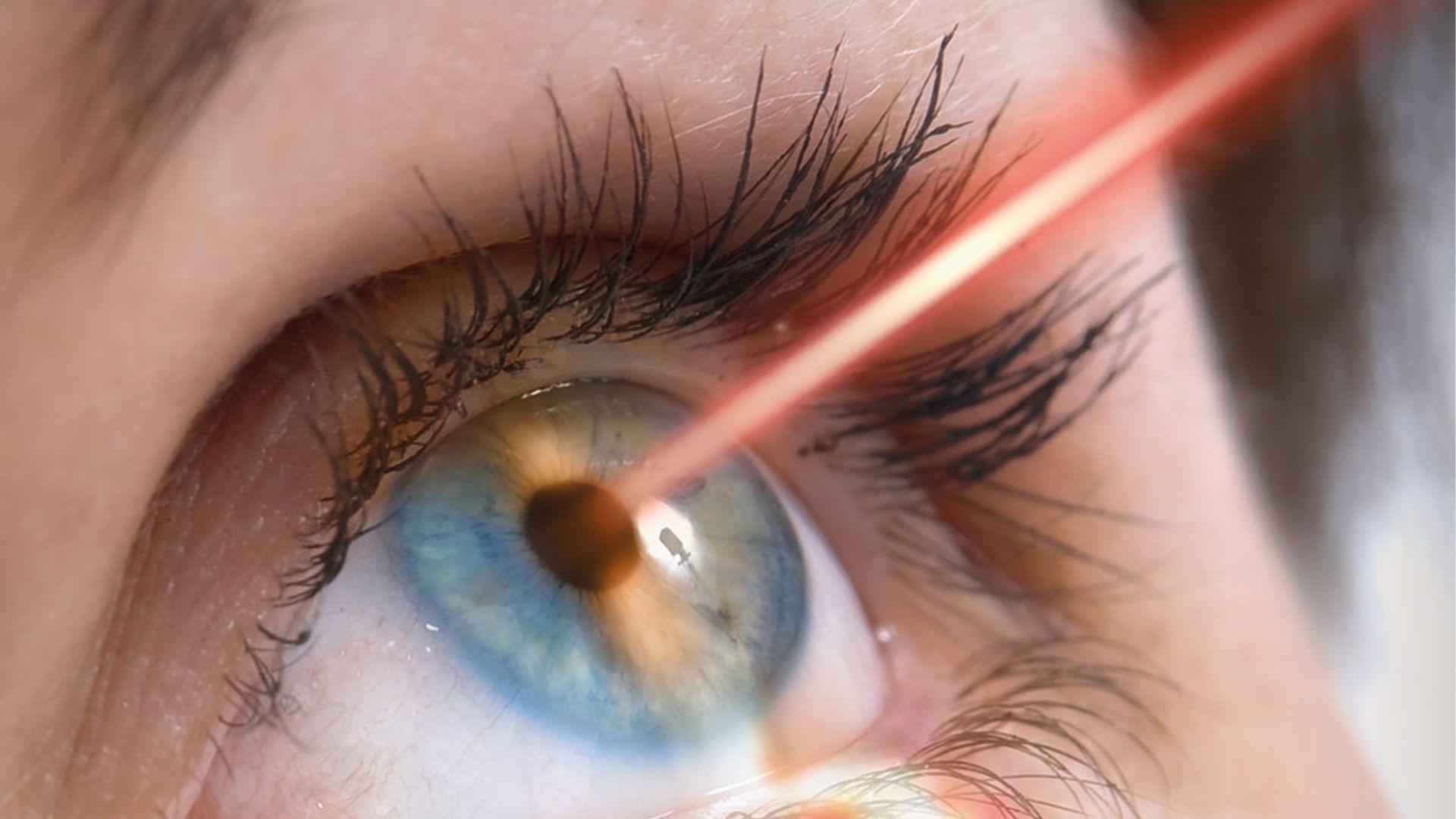
A beam of light is used to create tiny burns inside the eye during laser treatment, also known as photocoagulation. Edema and leaky blood vessels are treated using this approach. This therapy is typically given during several office visits, with an eye-numbing medicine being used to numb your eyes. Laser treatment has a greater chance of bringing diabetic retinopathy under control than other diabetic eye diseases.
There are two distinct forms of laser therapy.
- Diabetic macular edema is treated using a laser treatment called Focal/grid laser therapy, which targets a tiny part of the retina.
- Scatter laser therapy (pan-retinal photocoagulation) treats a larger area of the eye. This method aims to stop the formation of aberrant blood vessels known as proliferative diabetic retinopathy
Vitrectomy
A vitrectomy is a surgical procedure to remove the clear gel that fills the center of the eye, called the vitreous gel. Proliferative diabetic retinopathy may lead to severe bleeding or scar tissue, which can be treated with this surgery. Scar tissue might push against the retina and cause it to peel away from the underlying tissue.
A vitrectomy is also performed on diabetic eye disease patients who have severe bleeding that cannot be controlled with other surgical procedures. A gas bubble injected into the eye can keep the retina from re-attaching to the wall of your eyeball during recovery. This procedure is pars plana vitrectomy, and it may increase your chances of being able to preserve your vision.
A clear salt solution is gently infused into the eye during vitrectomy to maintain eye pressure and replace the removed vitreous. Vitrectomy is performed in a surgery center or hospital, where appropriate pain medication is given.
Cataract Lens Surgery
Your doctor may remove the hazy lens in your eye, where the cataract has developed, and replace it with an artificial lens during a surgery center or hospital visit. Cataract surgery generally leads to improved vision. Following cataract surgery, you might require a new pair of glasses prescription.
Prevention
Keep an eye on your A1c, blood pressure, and cholesterol levels; and quit smoking if you smoke to avoid diabetic eye disease or to help it from getting worse. Manage your diabetes ABCs: your A1c, blood pressure, and cholesterol; and quit smoking if you do.
Have an eye doctor check your eyes at least once a year, or more frequently if recommended by your eye care professional. These techniques are beneficial in preserving the health of your eyes and preventing blindness.
The sooner you start working to manage your diabetes and other health issues, the better. Taking better care of yourself now can help you preserve your eyes for the future, even if you’ve had trouble in the past managing your health. It’s never too late to make a change.
Conclusion
Now that you know more about diabetic eye disease, it’s important to take care of your eyes. Take a few moments each day for dry-eye relief and have an annual comprehensive examination with your optometrist or ophthalmologist if you’re at risk. You can also help prevent the onset of this condition by maintaining a healthy lifestyle and eating a balanced diet full of fresh fruits and vegetables as well as whole grains. If any questions come up, make sure to talk with your doctor right away! With proper treatment from an experienced professional, there is hope for those suffering from diabetic eye disease.
Do you want to get rid of diabetes? Join our online diabetes consultation program and reverse your Diabetes naturally through lifestyle changes such as a Personalized Diet plan, Exercise, dieticians, and health coaches.