Obsessive-Compulsive Disorder (OCD) is a challenging mental health condition that can severely impact daily functioning and quality of life. While traditional treatments like psychotherapy and medications are effective for many, some individuals continue to struggle with persistent symptoms. In recent years, Deep Brain Stimulation (DBS) has emerged as a groundbreaking alternative for treatment-resistant OCD. So, here we will delve into the mechanisms, effectiveness, and risks associated with DBS for OCD.
Contents
Does DBS Help With OCD?
 Yes, Deep Brain Stimulation (DBS) has shown promise in helping individuals with severe Obsessive-Compulsive Disorder (OCD) who have not responded to conventional treatments. DBS involves surgically implanting electrodes in specific areas of the brain associated with OCD symptoms. These electrodes emit electrical impulses that regulate abnormal impulses that may contribute to OCD symptoms.
Yes, Deep Brain Stimulation (DBS) has shown promise in helping individuals with severe Obsessive-Compulsive Disorder (OCD) who have not responded to conventional treatments. DBS involves surgically implanting electrodes in specific areas of the brain associated with OCD symptoms. These electrodes emit electrical impulses that regulate abnormal impulses that may contribute to OCD symptoms.
Clinical trials and research studies have demonstrated that DBS can significantly reduce symptoms for many patients. And, leading to substantial improvements in their quality of life. However, DBS is considered an invasive procedure and is typically reserved for cases where all other treatments have failed. The effectiveness of DBS can vary from person to person, and the procedure carries potential risks and side effects.
How Does DBS For OCD Work?
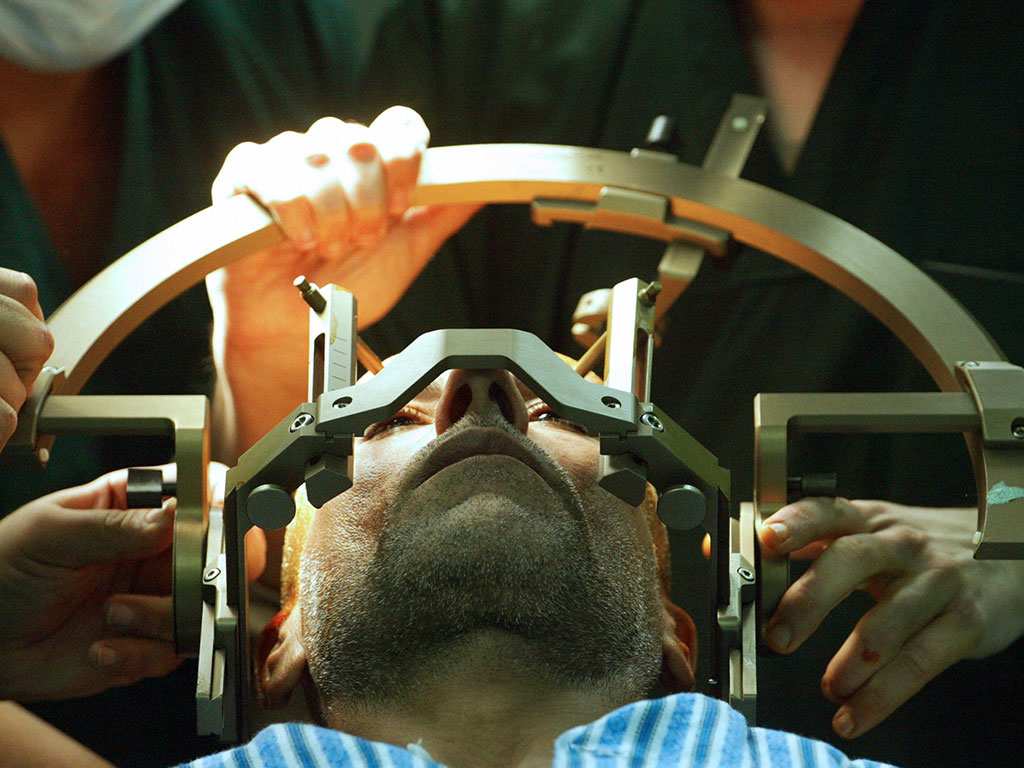
Deep Brain Stimulation (DBS) for Obsessive-Compulsive Disorder (OCD) is a neurosurgical procedure that involves the implantation of electrodes in specific areas of the brain that are known to be involved in OCD. The process targets the neural circuits that are believed to malfunction in OCD, aiming to alter the abnormal activity that contributes to the symptoms.
Here’s a step-by-step overview of how DBS works for OCD:
Target Identification
The first step in DBS therapy is to identify the precise areas of the brain that are involved in the patient’s OCD symptoms. Common targets for OCD include the ventral capsule/ventral striatum (VC/VS), which is part of the circuitry that affects emotional regulation and response to fear, and the subthalamic nucleus. This is involved in motor control and impulsive behaviors.
Surgical Implantation
During the surgery, electrodes are carefully implanted in the targeted brain areas. This procedure is typically done under local anesthesia and involves using magnetic resonance imaging (MRI) or computed tomography (CT) scans to guide the placement of the electrodes accurately.
Device Configuration
The electrodes are connected by wires to a neurostimulator, a small battery-powered device similar to a pacemaker, which is usually implanted under the skin in the chest. The neurostimulator sends electrical impulses through the electrodes to the brain.
Stimulation Adjustment
After implantation, the device is programmed and adjusted by a specialist. This involves fine-tuning the frequency, intensity, and duration of the electrical impulses. The goal is to find the settings that best reduce OCD symptoms without causing undesirable side effects.
Continuous Monitoring and Adjustment
The settings of the DBS device can be adjusted over time as the patient’s condition changes or in response to any side effects. Regular follow-ups are necessary to monitor the effectiveness of the therapy and the overall well-being of the patient.
DBS works by modulating the electrical and chemical activity within specific brain circuits, potentially “resetting” the brain areas involved in OCD. While the exact mechanism is not fully understood, it is thought that DBS helps to normalize the signals in these circuits, thereby reducing the intensity of OCD symptoms.
What Are The Benefits You Can Expect?
 DBS for OCD can offer significant benefits, especially for individuals who have not found relief from traditional treatments like medication and psychotherapy. Here are some of the primary benefits:
DBS for OCD can offer significant benefits, especially for individuals who have not found relief from traditional treatments like medication and psychotherapy. Here are some of the primary benefits:
- Improvement in Quality of Life
With a decrease in symptoms, patients often report an overall improvement in quality of life. This includes better social interactions, improved performance at work or school, and a greater ability to engage in leisure activities that were previously hindered by OCD symptoms.
- Customizable Treatment
DBS settings can be adjusted and tailored to the individual needs of the patient. This means that the therapy can be optimized over time to maximize benefits and minimize side effects.
- Reversible and Adjustable
Unlike some other surgical interventions, DBS is both reversible and adjustable. If necessary, the system can be turned off or removed, and the stimulation settings can be changed depending on the patient’s response to the therapy.
- Psychological Benefits
Reduction in OCD symptoms can also lead to improved mental health overall. Patients may experience decreases in associated conditions such as anxiety and depression, further contributing to an enhanced quality of life.
- Safety Track Record
Although DBS is a significant procedure, it has been used safely for decades in the treatment of other neurological disorders such as Parkinson’s disease. This provides a basis for its safety and efficacy in treating psychiatric disorders like OCD.
It’s important for patients considering DBS to discuss these potential benefits with their healthcare providers, as well as the risks and commitment involved. Proper patient selection and expert handling are crucial for maximizing the positive outcomes of DBS therapy.
What Are The Risks And Considerations Of DBS For OCD?
DBS for OCD is a sophisticated and invasive treatment option that carries certain risks and considerations. While DBS can be life-changing for some, patients and their families need to weigh these factors carefully:
Risks Associated with Surgery
- Infection: As with any surgical procedure, there is a risk of infection at the site of the surgery or in the brain, although strict surgical protocols minimize this risk.
- Bleeding in the Brain: There is a small risk of bleeding in the brain during electrode placement. This can lead to stroke-like symptoms or other neurological impairments.
- Hardware Complications: Problems can occur with the implanted device, such as malfunctions or displacement of the electrodes. It might require additional surgeries.
Neurological and Psychological Effects
- Unwanted Side Effects: Stimulation can sometimes affect areas of the brain involved in mood and cognition, potentially causing side effects like apathy, hallucinations, heightened anxiety, or mood changes.
- Adjustment Period: It can take time to find the optimal stimulation settings. During this period, patients may experience varying levels of symptom relief and side effects.
Long-term Considerations
- Dependency on the Device: DBS is not a cure for OCD and typically requires lifelong management. The neurostimulator may need battery replacements or other maintenance surgeries over time.
- Reversibility: While DBS is reversible in the sense that the device can be turned off or removed, any changes to brain tissue caused by the electrodes are permanent.
Financial and Accessibility Issues
- Cost: DBS is a costly procedure that includes expenses for the surgery, the device, and ongoing adjustments and maintenance. Insurance coverage varies, and not all patients may have access to such resources.
- Availability: Access to DBS treatment is limited to specialized medical centers with the necessary expertise. Potentially limiting availability for those in less-served regions.
Given these risks and considerations, DBS is typically reserved for patients with severe, treatment-resistant OCD who have exhausted other therapeutic options. Hence, patients need to engage in detailed discussions with a multidisciplinary team of specialists to understand the potential risks and benefits thoroughly.
How Much Does Deep Brain Stimulation Cost?
 The cost of Deep Brain Stimulation (DBS) can vary widely depending on several factors, including the healthcare system, the specific hospital or clinic, geographical location, and the individual patient’s medical needs. In the United States, the total cost of DBS surgery can range from $30,000 to $100,000. This includes the cost of the surgical procedure, the neurostimulator device itself, and the associated hospital stay.
The cost of Deep Brain Stimulation (DBS) can vary widely depending on several factors, including the healthcare system, the specific hospital or clinic, geographical location, and the individual patient’s medical needs. In the United States, the total cost of DBS surgery can range from $30,000 to $100,000. This includes the cost of the surgical procedure, the neurostimulator device itself, and the associated hospital stay.
However, the initial surgery cost is just part of the overall financial commitment. Patients will also incur costs for pre-surgical assessments, follow-up adjustments, maintenance, and potential replacement of the neurostimulator battery.
Patients considering DBS should consult with their insurance providers to understand what parts of the procedure and follow-up care are covered. And to assess any out-of-pocket expenses. Additionally, financial assistance programs may be available through hospitals or charitable organizations.
Conclusion
In conclusion, Deep Brain Stimulation (DBS) represents a significant advancement in treating severe, treatment-resistant Obsessive-Compulsive Disorder (OCD). While it offers a chance for substantial relief from the debilitating symptoms of OCD, DBS involves complex surgery and carries potential risks. The procedure is costly. But also requires ongoing adjustments and lifelong management.
Therefore, this treatment should be seen as a last resort, pursued only after traditional treatments have proven ineffective. Take care, and don’t forget that you are not alone! If you have any queries regarding OCD treatment, ERP therapy experienced therapists at OCDMantra can help: Book a trial OCD therapy session